74 articles scientifiques sur le syndrome de Dravet parus en 2012. Ci-après leur résumé.
Bonne lecture !
Zhonghua Yi Xue Yi Chuan Xue Za Zhi. 2012 Dec;29(6):625-30. doi: 10.3760/cma.j.issn.1003-9406.
[Genetic and phenotypic characteristics of SCN1A mutations in Dravet syndrome].
[Article in Chinese]
Xu XJ, Zhang YH, Sun HH, Liu XY, Jiang YW, Wu XR.
Department of Pediatrics, Peking University First Hospital, Beijing 100034, P R China.
OBJECTIVE:
To study SCN1A gene mutations and their inheritance in patients with Dravet syndrome(DS), and to analyze the phenotypes of their family members and genotype-phenotype correlations.
METHODS:
Genomic DNA was extracted from peripheral blood samples from 181 DS patients and their parents. Phenotypes of affected members were analyzed. SCN1A gene mutations were screened using PCR-DNA sequencing and multiplex ligation-dependent probe amplification (MLPA) RESULTS: SCN1A gene mutations were identified in 128 patients (70.7%), which included 60 missense mutations (46.9%), 55 truncation mutations (43.0%), 10 splice site mutations (7.8%), and 3 cases with SCN1A gene fragment deletions or duplications(2.3%). Five patients (3.9%) had mutations inherited from one of their parents. One father has carried a somatic mutation mosaicism (C373fsx378). For the 5 parents carrying a mutation, 1 had febrile seizures, 2 had febrile seizures plus, 1 had afebrile generalized tonic-clonic seizures, whilst 1 was normal.
CONCLUSION:
The mutation rate of SCN1A in DS patients is about 70%. Most mutations are of missense and truncation mutations. Only a few patients have carried fragment deletions or duplications. Most SCN1A mutations are de novo, only a few were inherited from the parents. SCN1A mutations carried by the parents can be in the form of mosaicism. The phenotypes of parents with SCN1A mutations are either mild or normal.
Epilepsy Res Treat. 2012;2012:403592. doi: 10.1155/2012/403592. Epub 2012 Nov 20.
Epileptic encephalopathies: an overview.
Khan S, Al Baradie R.
Department of Clinical Neurosciences, Prince Sultan Military Medical City, P.O. Box 7897, Riyadh 11159, Saudi Arabia.
Epileptic encephalopathies are an epileptic condition characterized by epileptiform abnormalities associated with progressive cerebral dysfunction. In the classification of the International League Against Epilepsy eight age-related epileptic encephalopathy syndromes are recognized. These syndromes include early myoclonic encephalopathy and Ohtahara syndrome in the neonatal period, West syndrome and Dravet syndrome in infancy, myoclonic status in nonprogressive encephalopathies, and Lennox-Gastaut syndrome, Landau-Kleffner syndrome, and epilepsy with continuous spike waves during slow wave sleep in childhood and adolescences. Other epileptic syndromes such as migrating partial seizures in infancy and severe epilepsy with multiple independent spike foci may be reasonably added. In this paper, we provide an overview of epileptic encephalopathies including clinical neurophysiological features, cognitive deterioration, and management options especially that these conditions are generally refractory to standard antiepileptic drugs.
Eur Neurol. 2013;69(2):119-21. doi: 10.1159/000345132. Epub 2012 Nov 29.
Effect of vagus nerve stimulation in an adult patient with dravet syndrome: contribution to sudden unexpected death in epilepsy risk reduction?.
Spatola M, Jeannet PY, Pollo C, Wider C, Labrum R, Rossetti AO.
Service de Neurologie, Centre Hospitalier Universitaire Vaudois and University of Lausanne, Lausanne, Switzerland.
We report on a patient who developed, from 5 months of age, multiple seizure types, including myoclonic, associated with severe psychomotor delay, leading to the diagnosis of Dravet syndrome. Over the years, he developed refractory epilepsy and was implanted with a vagus nerve stimulator at the age of 19. After 3 months, he experienced a progressive improvement of partial and generalized seizures, with a >90% reduction, and better alertness. This meaningful clinical improvement is discussed in the light of the sudden unexpected death in epilepsy risk, which is high in this setting, and seems remarkably diminished in our patient in view of the reduction of generalized convulsions.
Epilepsy Res. 2012 Dec;102(3):195-200. doi: 10.1016/j.eplepsyres.2012.06.
Prevalence of SCN1A mutations in children with suspected Dravet syndrome and intractable childhood epilepsy.
Wang JW, Shi XY, Kurahashi H, Hwang SK, Ishii A, Higurashi N, Kaneko S, Hirose S; Epilepsy Genetic Study Group Japan.
Department of Pediatrics, School of Medicine, Central Research Institute for the Pathomechanisms of Epilepsy, Fukuoka University, Fukuoka, Japan.
Mutations of the gene encoding the α1 subunit of neuronal sodium channel, SCN1A, are reported to cause Dravet syndrome (DS). The prevalence of mutations reported in such studies (mainly in clinically confirmed DS) seems high enough to make genetic diagnosis feasible. In fact, commercially operating genetic diagnostic laboratories offering genetic analyses of SCN1A are available. Still, the exact prevalence of mutations of SCN1A remains elusive. Fukuoka University has been serving as a genetic diagnostic laboratory for DS for the last 10 years. In this study, we determined the prevalence of SCN1A mutations (SCN1A, SCN2A, SCN1B and SCN2B) in 448 patients with suspected DS and intractable childhood epilepsy. A total of 192 SCN1A mutations were identified in 188 of 448 patients (42.0%). The frequencies of SCN1A mutations in suspected severe myoclonic epilepsy of infancy (SMEI), its borderline phenotype (SMEB) and intractable epilepsy were 56.2%, 41.9% and 28.9% respectively. In addition, four SCN2A mutations were identified in 4 of 325 patients. No mutations of SCN1B and SCN2B were identified. These results are potentially helpful for the diagnosis of DS at early stage.
Epilepsy Res. 2013 Jan;103(1):97-100. doi: 10.1016/j.eplepsyres.2012.10.
Do mutations in SCN1B cause Dravet syndrome?
Kim YO, Dibbens L, Marini C, Suls A, Chemaly N, Mei D, McMahon JM, Iona X, Berkovic SF, De Jonghe P, Guerrini R, Nabbout R,Scheffer IE.
Epilepsy Research Centre, Department of Medicine, The University of Melbourne, Austin Health, Melbourne, Australia.
A homozygous SCN1B mutation was previously identified in a patient with early onset epileptic encephalopathy (EOEE) described as Dravet syndrome (DS) despite a more severe phenotype than DS. We investigated whether SCN1B mutations are a common cause of DS. Patients with DS who did not have a SCN1A sequencing mutation or copy number variation were studied. Genomic DNA was Sanger sequenced for mutations in the 6 exons of SCN1B. In 54 patients with DS recruited from four centres, no SCN1B mutations were identified. SCN1B mutation is not a common cause of DS.
Neuropharmacology. 2013 Apr;67:136-43. doi: 10.1016/j.neuropharm.2012.11.
Stiripentol is anticonvulsant by potentiating GABAergic transmission in a model of benzodiazepine-refractory status epilepticus.
Grosenbaugh DK, Mott DD.
Department of Pharmacology, Physiology and Neuroscience, University of South Carolina, School of Medicine, Columbia, SC 29208, USA. Denise.Grosenbaugh@uscmed.sc.
Benzodiazepines (BZDs) are first-line therapy for treatment of status epilepticus (SE). However, BZD treatment is negatively affected by seizure duration due to decreases in BZD-sensitive GABA(A) receptors during prolonged SE. Stiripentol (STP) is an anticonvulsant that is used as add-on treatment for Dravet Syndrome. Recent studies have shown that STP is a positive allosteric modulator of the GABA(A) receptor. The subunit selectivity of STP at this receptor suggests that it would be anticonvulsant in both brief as well as prolonged SE. We tested this possibility by comparing the ability of STP and diazepam (DZP), a commonly used BZD, to terminate behavioral convulsions in a rodent model of pharmacoresistant SE. We found that STP was anticonvulsant in this model and remained effective during prolonged SE, unlike DZP which exhibited a 14 fold increase in its ED(50). Whole cell recording from hippocampal slices from these animals revealed that STP potentiated GABAergic IPSCs, as well as tonic GABAergic current by acting at a site on the GABA(A) receptor separate from the BDZ binding site. Potentiation of GABAergic currents by STP remained intact during prolonged SE, while potentiation by DZP was lost. Both IPSC potentiation and anticonvulsant activity of STP were greater in younger animals than in adults. These findings suggest that at doses that yield therapeutically relevant concentrations, STP is anticonvulsant by potentiating GABAergic inhibition and that the subunit selectivity profile of STP enables it to remain effective despite GABA(A) receptor subunit changes during prolonged SE.
Dev Med Child Neurol. 2013 Feb;55(2):154-61. doi: 10.1111/dmcn.12030. Epub 2012 Nov 20.
The clinical utility of an SCN1A genetic diagnosis in infantile-onset epilepsy.
Brunklaus A, Dorris L, Ellis R, Reavey E, Lee E, Forbes G, Appleton R, Cross JH, Ferrie C, Hughes I, Jollands A, King MD,Livingston J, Lynch B, Philip S, Scheffer IE, Williams R, Zuberi SM.
The Paediatric Neurosciences Research Group, Royal Hospital for Sick Children, Glasgow, UK.
Comment in
- Genetic testing improves care for infantile-onset epilepsy: the story of SCN1A. [Dev Med Child Neurol. 2013]
Genetic testing improves care for infantile-onset epilepsy: the story of SCN1A.Berg AT. Dev Med Child Neurol. 2013 Feb; 55(2):102-3. Epub 2012 Nov 27.
AIM:
Genetic testing in the epilepsies is becoming an increasingly accessible clinical tool. Mutations in the sodium channel alpha 1 subunit (SCN1A) gene are most notably associated with Dravet syndrome. This is the first study to assess the impact of SCN1A testing on patient management from both carer and physician perspectives.
METHOD:
Participants were identified prospectively from referrals to the Epilepsy Genetics Service in Glasgow and contacted via their referring clinicians. Questionnaires exploring the consequences of SCN1A genetic testing for each case were sent to carers and physicians.
RESULTS:
Of the 244 individuals contacted, 182 (75%) carried a SCN1A mutation. Carers of 187 (77%) patients responded (90 females, 97 males; mean age at referral 4 y 10 mo; interquartile range 9 y 1 mo). Of those participants whose children tested positive for a mutation, 87% reported that genetic testing was helpful, leading to treatment changes resulting in fewer seizures and improved access to therapies and respite care. Out of 187 physicians, 163 responded (87%), of whom 48% reported that a positive test facilitated diagnosis earlier than with clinical and electroencephalography data alone. It prevented additional investigations in 67% of patients, altered treatment approach in 69%, influenced medication choice in 74%, and, through medication change, improved seizure control in 42%.
INTERPRETATION:
In addition to confirming a clinical diagnosis, a positive SCN1A test result influenced treatment choice and assisted in accessing additional therapies, especially in the very young.
Zhonghua Er Ke Za Zhi. 2012 Aug;50(8):580-6.
[Phenotype and SCN1A gene mutation screening in 39 families with generalized epilepsy with febrile seizures plus].
[Article in Chinese]
Xu XJ, Zhang YH, Sun HH, Liu XY, Wu HS, Wu XR.
Department of Pediatrics, First Hospital, Peking University, Beijing, China.
OBJECTIVE:
To summarize the phenotypes and identify SCN1A mutations in families with generalized epilepsy with febrile seizures plus (GEFS(+)), and analyze the genotype- phenotype correlations in GEFS(+) families.
METHOD:
Genomic DNA was extracted from peripheral blood lymphocytes of the proband and other available members in the GEFS(+) families. The phenotypes of the affected members were analyzed. The coding regions and flanking intronic regions of the SCN1A gene were screened for mutations using PCR and direct DNA sequencing.
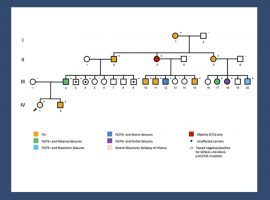
RESULT:
In 39 GEFS(+) families, there were 196 affected members, ranging from 2 to 22 affected members in each family. Their phenotypes included febrile seizures (FS) in 92(46.9%), febrile seizures plus (FS(+)) in 62(31.6%), FS or FS(+) with partial seizures in 12(6.1%), afebrile generalized tonic-clonic seizures (AGTCS) in 11(5.6%), myoclonic atonic epilepsy in 8(4.1%), Dravet syndrome in 2(1.0%), childhood absence epilepsy in 1 (0.5%), FS(+) with myoclonic seizures in 1(0.5%), AGTCS and myoclonic seizures in 1 (0.5%), partial seizures in 1 (0.5%), unclassified seizures in 5 (2.6%). Four families were found with SCN1A mutations, including three families with missense mutation (N935H, R101Q, G1382R) and one family with truncation mutation (C373fsx378). In three families with missense mutations, the phenotypes include FS, FS(+), FS(+) with partial seizures, and AGTCS. In one family with truncation mutation, the phenotypes included FS, FS(+), and Dravet syndrome. The mother of proband in the family with missense mutation (R101Q) and the father of proband in the family with truncation mutation (C373fsx378) were both somatic mosaicism. Both of their phenotypes were FS(+).
CONCLUSION:
The most common phenotypes of GEFS(+) were FS and FS(+), followed by the FS/FS(+) with partial seizures and AGTCS. The most severe phenotype was Dravet syndrome. SCN1A mutation rate in GEFS(+) was about 10%. Missense mutation was common in GEFS(+) families, few with truncation mutation. Few members of GEFS(+) families had somatic mosaicism of SCN1A mutations and their phenotypes were relatively mild.
Epilepsia. 2012 Dec;53(12):e200-3. doi: 10.1111/epi.12040. Epub 2012 Nov 13.
A homozygous mutation of voltage-gated sodium channel β(I) gene SCN1B in a patient with Dravet syndrome.
Ogiwara I, Nakayama T, Yamagata T, Ohtani H, Mazaki E, Tsuchiya S, Inoue Y, Yamakawa K.
Laboratory for Neurogenetics, RIKEN Brain Science Institute, Wako, Saitama, Japan.
Dravet syndrome is a severe form of epileptic encephalopathy characterized by early onset epileptic seizures followed by ataxia and cognitive decline. Approximately 80% of patients with Dravet syndrome have been associated with heterozygous mutations in SCN1A gene encoding voltage-gated sodium channel (VGSC) α(I) subunit, whereas a homozygous mutation (p.Arg125Cys) of SCN1B gene encoding VGSC β(I) subunit was recently described in a patient with Dravet syndrome. To further examine the involvement of homozygous SCN1B mutations in the etiology of Dravet syndrome, we performed mutational analyses on SCN1B in 286 patients with epileptic disorders, including 67 patients with Dravet syndrome who have been negative for SCN1A and SCN2A mutations. In the cohort, we found one additional homozygous mutation (p.Ile106Phe) in a patient with Dravet syndrome. The identified homozygous SCN1B mutations indicate that SCN1B is an etiologic candidate underlying Dravet syndrome.
Neurobiol Dis. 2013 Feb;50:209-17. doi: 10.1016/j.nbd.2012.10.016. Epub 2012 Oct 25.
CACNA1A variants may modify the epileptic phenotype of Dravet syndrome.
Ohmori I, Ouchida M, Kobayashi K, Jitsumori Y, Mori A, Michiue H, Nishiki T, Ohtsuka Y, Matsui H.
Department of Physiology, Graduate School of Medicine, Dentistry and Pharmaceutical Sciences, Okayama University, Shikatacho 2-chome 5-1, Kita-ku, Okayama 700-8558, Japan. iori@md.okayama-u.ac.jp
Dravet syndrome is an intractable epileptic syndrome beginning in the first year of life. De novo mutations of SCN1A, which encode the Na(v)1.1 neuronal voltage-gated sodium channel, are considered the major cause of Dravet syndrome. In this study, we investigated genetic modifiers of this syndrome. We performed a mutational analysis of all coding exons of CACNA1A in 48 subjects with Dravet syndrome. To assess the effects of CACNA1A variants on the epileptic phenotypes of Dravet syndrome, we compared clinical features in two genotype groups: 1) subjects harboring SCN1A mutations but no CACNA1A variants (n=20) and 2) subjects with SCN1A mutations plus CACNA1A variants (n=20). CACNA1A variants detected in patients were studied using heterologous expression of recombinant human Ca(v)2.1 in HEK 293 cells and whole-cell patch-clamp recording. Nine CACNA1A variants, including six novel ones, were detected in 21 of the 48 subjects (43.8%). Based on the incidence of variants in healthy controls, most of the variants seemed to be common polymorphisms. However, the subjects harboring SCN1A mutations and CACNA1A variants had absence seizures more frequently than the patients with only SCN1A mutations (8/20 vs. 0/20, p=0.002). Moreover, the former group of subjects exhibited earlier onset of seizures and more frequent prolonged seizures before one year of age, compared to the latter group of subjects. The electrophysiological properties of four of the five novel Ca(v)2.1 variants exhibited biophysical changes consistent with gain-of-function. We conclude that CACNA1A variants in some persons with Dravet syndrome may modify the epileptic phenotypes.
Acta Med Okayama. 2012;66(5):369-76.
Dravet syndrome: a genetic epileptic disorder.
Akiyama M, Kobayashi K, Ohtsuka Y.
Department of Child Neurology, Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Sciences, and Okayama University Hospital, Okayama 700-8558, Japan. akiyamama@s-okayama.hosp.go.jp
Dravet syndrome (DS), or severe myoclonic epilepsy in infancy, is one of the most severe types of genetic epilepsy. It is characterized by the initial occurrence of febrile or afebrile seizures that often evolve into status epilepticus in infants with normal development, and by the subsequent appearance of myoclonic and/or atypical absence seizures as well as complex partial seizures. The key feature that characterizes DS is fever sensitivity, although photosensitivity and pattern-sensitivity are also often seen. The prognosis is unfavorable in most cases. Seizures become drug-resistant and persist, with many patients suffering from motor and cognitive impairment. Mutations of SCN1A, which encodes the voltage-gated sodium channel NaV1.1, are the most frequent genetic cause of this syndrome. SCN1A mutations and/or microchromosomal rearrangements involving SCN1A are detected in about 85オ of patients. Mutations of PCDH19 have also been reported in female patients with clinical findings compatible with DS. PCDH19 mutations might account for 5オ of overall DS cases. Thirty years after its first description, DS is considered as a model of channelopathy. This survey reviews recent developments in the research literature on DS, focusing on the clinical course, as well as its genetic causes.
J Biol Chem. 2012 Dec 7;287(50):42001-8. doi: 10.1074/jbc.M112.421883. Epub 2012 Oct 19.
Nontruncating SCN1A mutations associated with severe myoclonic epilepsy of infancy impair cell surface expression.
Thompson CH, Porter JC, Kahlig KM, Daniels MA, George AL Jr.
Department of Medicine, Vanderbilt University, Nashville, Tennessee 37232, USA.
Mutations in SCN1A, encoding the voltage-gated sodium channel Na(V)1.1, are the most common cause of severe myoclonic epilepsy of infancy (SMEI) or Dravet syndrome. SMEI is most often associated with premature truncations of Na(V)1.1 that cause loss of function, but nontruncating mutations also occur. We hypothesized that some nontruncating mutations might impair trafficking of Na(V)1.1 to the plasma membrane. Here we demonstrated that seven nontruncating missense or in-frame deletion mutations (L986F, delF1289, R1648C, F1661S, G1674R, and G1979E) exhibited reduced cell surface expression relative to wild type (WT) Na(V)1.1 consistent with impaired trafficking. We tested whether two commonly prescribed antiepileptic drugs (phenytoin, lamotrigine), as well as the cystic fibrosis transmembrane conductance regulator (CFTR) trafficking corrector VRT-325, could rescue cell surface and functional expression of two representative Na(V)1.1 mutants (R1648C, G1674R). Treatment of cells with phenytoin increased cell surface expression of WT-Na(V)1.1 and both mutant channels, whereas lamotrigine only increased surface expression of R1648C. VRT-325 did not alter surface expression of WT-Na(V)1.1 or mutant channels. Although phenytoin increased surface expression of G1674R, channel function was not restored, suggesting that this mutation also causes an intrinsic loss of function. Both phenytoin and lamotrigine increased functional expression of R1648C, but lamotrigine also increased persistent sodium current evoked by this mutation. Our findings indicate that certain nontruncating SCN1A mutations associated with SMEI have impaired cell surface expression and that some alleles may be amenable to pharmacological rescue of this defect. However, rescue of dysfunctional Na(V)1.1 channels to the plasma membrane could contribute to exacerbating rather than ameliorating the disease.
Neurobiol Dis. 2013 Feb;50:135-41. doi: 10.1016/j.nbd.2012.10.008. Epub 2012 Oct 13.
Impaired surface αβγ GABA(A) receptor expression in familial epilepsy due to a GABRG2 frameshift mutation.
Tian M, Mei D, Freri E, Hernandez CC, Granata T, Shen W, Macdonald RL, Guerrini R.
Department of Neurology, Vanderbilt University Medical Center, Nashville, TN 37212, USA. mengnan.tian@vanderbilt.edu
The purpose of the study was to explore the pathogenic mechanisms underlying generalized epilepsy and febrile seizures plus (GEFS+) in a family with a novel γ2 subunit gene (GABRG2) frameshift mutation. Four affected and one unaffected individuals carried a c.1329delC GABRG2 mutation resulting in a subunit [γ2S(S443delC)] with a modified and elongated carboxy-terminus that is different from that of the wildtype γ2S subunit. We expressed the wildtype γ2S subunit and the predicted mutant γ2S(S443delC) subunit cDNAs in HEK293T cells and performed immunoblotting, flow cytometry and electrophysiology studies. The mutant subunit was translated as a stable protein that was larger than the wildtype γ2S subunit and was retained in the ER and not expressed on the cell surface membrane, suggesting GABRG2 haploinsufficiency. Peak GABA-evoked currents recorded from cells cotransfected with wildtype α1 and β2 subunits and mutant γ2S subunits were significantly decreased and were comparable to α1β2 receptor currents. S443delC is the first GABR epilepsy mutation predicted to abolish the natural stop codon and produce a stop codon in the 3′ UTR that leads to translation of an extended peptide. The GEFS+ phenotype observed in this family is likely caused by γ2S subunit loss-of-function and possibly to dominant-negative suppression of α1β2γ2 receptors. Many GABRG2 truncation mutations result in GEFS+, but the spectrum of phenotypic severity is wider, ranging from asymptomatic individuals to the Dravet syndrome. Mechanisms influencing the severity of the phenotype are therefore complex and difficult to correlate with its demonstrable functional effects.
Acta Neurol Belg. 2013 Jun;113(2):161-6. doi: 10.1007/s13760-012-0140-z. Epub 2012 Oct 13
Dispersion de l’onde P et de l’intervalle QT et variabilité de la fréquence cardiaque chez des patients atteints du syndrome de Dravet.
Ergul Y, Ekici B, Tatli B, Nisli K, Ozmen M.
Département de Cardiologie pédiatrique, Faculté de Médecine d’Istanbul, Université d’Istanbul, Istanbul, Turquie. yakupergul77@hotmail.com
Des mutations du gène SCN1A sont détectées chez près de 80 % des patients présentant un syndrome de Dravet (SD) et le taux de mort subite inexpliquée dans l’épilepsie (SUDEP) est plus élevé dans le SD que dans la plupart des formes d’épilepsie sévère. L’objectif de cette étude était d’examiner la fonction cardiaque autonome et le risque d’arythmies chez des patients atteints du SD en évaluant la dispersion de l’onde P et de l’intervalle QT et la variabilité de la fréquence cardiaque (VFC) par électrocardiographie (ECG) standard et monitorage ECG sur 24 heures. Le groupe étudié était composé de 15 patients (9 garçons et 6 filles âgés de 3,5 à 17 ans) ayant un diagnostic génétique de syndrome de Dravet. Le groupe témoin était composé de 20 sujets sains, 13 garçons et 7 filles âgés de 4 à 17 ans. La dispersion de l’onde P (44,6 ± 3,5 ms), la dispersion de l’intervalle QT (58,8 ± 7,5 ms) et la dispersion de l’intervalle QTc (70,8 ± 7,4 ms) ont été significativement supérieures chez les patients présentant un SD par rapport au groupe témoin (P < 0,001 pour toutes les valeurs). Cependant, il n’a pas été observé de différence significative entre les groupes dans la longueur des intervalles PR, QT ou QTc. Le Holter‑ECG sur 24 heures a montré que tous les paramètres de variabilité de la fréquence cardiaque étaient significativement plus faibles chez les patients atteints du SD. La diminution de la VFC et l’augmentation de la dispersion de l’onde P et de l’intervalle QT observées chez ces patients sont des signes importants de dysfonctionnement autonome avec augmentation du tonus adrénergique. Un monitorage ECG à long terme et des études prospectives de plus grande taille sont nécessaires pour déterminer si le dysfonctionnement autonome est corrélé à la SUDEP dans le syndrome de Dravet.
Neuropediatrics. 2013 Jun;44(3):155-8. doi: 10.1055/s-0032-1327772. Epub 2012 Oct 3.
Encéphalopathie associée à l’herpèsvirus humain de type 6 chez une enfant atteinte du syndrome de Dravet.
Hiraiwa‑Sofue A, Ito Y, Ohta R, Kimura H, Okumura A.
Service de Pédiatrie, Hiraiwa Hospital, Nagoya, Japon
Le syndrome de Dravet est caractérisé par des crises cloniques ou tonico‑cloniques généralisées et unilatérales qui surviennent pendant la première année de vie, puis par une épilepsie sévère. Les crises convulsives prolongées sont souvent provoquées par la fièvre et généralement suivies d’une récupération à l’état antérieur. Nous décrivons le cas d’une fillette âgée de 13 mois atteinte du syndrome de Dravet qui a présenté des séquelles neurologiques sévères secondaires à une encéphalopathie associée à l’herpèsvirus humain de type 6. Une évolution clinique biphasique a été observée, avec de la fièvre et des crises convulsives prolongées au début, puis des crises réfractaires aux médicaments antiépileptiques. Les taux sériques de cytokines pro‑inflammatoires et de métalloprotéase matricielle de type 9, qui ont été associées au développement de l’encéphalopathie aiguë, n’étaient pas significativement augmentés, ce qui semble indiquer que ces molécules n’étaient pas les principales causes de l’atteinte neurologique chez cette patiente. Une prédisposition aux crises convulsives due à une mutation du gène SCN1A peut plutôt avoir contribué à l’encéphalopathie aiguë chez notre patiente.
CNS Drugs. 2012 Nov;26(11):993-1001. doi: 10.1007/s40263-012-0004-3.
Stiripentol : in severe myoclonic epilepsy of infancy (dravet syndrome).
Plosker GL.
Adis, Mairangi Bay, North Shore, Private Bag, Auckland, New Zealand. CNS@adis.com
Stiripentol is an anticonvulsant used as adjunctive therapy with valproate and clobazam in the management of patients with severe myoclonic epilepsy of infancy (SMEI; Dravet syndrome), a rare form of epilepsy that develops in the first year of life and is subsequently associated with significant morbidity and mortality. Results of a randomized, double-blind trial, in which patients (≥3 years of age) whose SMEI was inadequately controlled with valproate and clobazam received adjunctive therapy with stiripentol or placebo for 2 months, showed a significantly higher response rate in the stiripentol group compared with the placebo group (71 % vs. 5 %; p < 0.0001; primary endpoint). Responders were defined as those patients who experienced a ≥50 % reduction in clonic or tonic-clonic seizure frequency during the second month of the double-blind period compared with baseline. Almost half of the stiripentol recipients were seizure free during this period compared with none in the placebo group. Stiripentol was also statistically superior to placebo for secondary efficacy outcomes in the randomized controlled trial, which included the median number of seizures during the second month of the double-blind period and the mean percentage change from baseline in seizure frequency. These results are supported by efficacy data from other studies in patients with SMEI treated with stiripentol as adjunctive therapy, including a long-term retrospective analysis, prospectively conducted open-label studies and a meta-analysis. Drowsiness, loss of appetite and weight loss are the most frequently reported adverse events with stiripentol, and the drug inhibits various cytochrome P450 isoenzymes, potentially leading to clinically significant drug interactions. Stiripentol is an important addition to the limited treatment options available for the management of patients with SMEI.
Epilepsia. 2012 Dec;53(12):2128-34. doi: 10.1111/j.1528-1167.2012.
Duplication of the sodium channel gene cluster on 2q24 in children with early onset epilepsy.
Goeggel Simonetti B, Rieubland C, Courage C, Strozzi S, Tschumi S, Gallati S, Lemke JR.
Division of Pediatric Neurology, Department of Pediatrics, Inselspital, University of Berne, Berne, Switzerland. barbara.goeggel-simonetti@
PURPOSE:
Sodium channel gene aberrations are associated with a wide range of seizure disorders, particularly Dravet syndrome. They usually consist of missense or truncating gene mutations or deletions. Duplications involving multiple genes encoding for different sodium channels are not widely known. This article summarizes the clinical, radiologic, and genetic features of patients with 2q24 duplication involving the sodium channel gene cluster.
METHODS:
A systematic review of the literature and report of two cases.
KEY FINDINGS:
Nine individuals with 2q24 duplication involving the sodium channel gene cluster are described (seven female, two male). All presented with severe seizures refractory to anticonvulsant drugs. Seizure onset was in the neonatal period in eight patients with SCN1A-involvement, in infancy in one patient with SCN2A and SCN3A, but no SCN1A involvement. Seizure activity decreased and eventually stopped at 5-20 months of age. Seizures recurred at the age of 3 years in the patient with SCN2A and SCN3A, but no SCN1A involvement. Eight patients had a poor neurodevelopmental outcome despite seizure freedom.
SIGNIFICANCE:
This article describes a distinct seizure disorder associated with a duplication of the sodium gene cluster on 2q24 described in otherwise healthy neonates and infants with severe, anticonvulsant refractory seizures and poor developmental outcome despite seizure freedom occurring at the age of 5-20 months.
Neurobiol Dis. 2012 Aug 16;49C:29-40. doi: 10.1016/j.nbd.2012.08.003. [Epub ahead of print]
Mouse with Na(v)1.1 haploinsufficiency, a model for Dravet syndrome, exhibits lowered sociability and learning impairment.
Ito S, Ogiwara I, Yamada K, Miyamoto H, Hensch TK, Osawa M, Yamakawa K.
Laboratory for Neurogenetics, RIKEN Brain Science Institute, 2-1 Hirosawa, Wako, Saitama 351-0198, Japan; Department of Pediatrics, Graduate School of Medicine, Tokyo Women’s Medical University, 8-1 Kawada-cho, Shinjuku, Tokyo 162-8666, Japan.
Dravet syndrome is an intractable epileptic encephalopathy characterized by early onset epileptic seizures followed by cognitive decline, hyperactivity, autistic behaviors and ataxia. Most Dravet syndrome patients possess heterozygous mutations of SCN1A gene encoding voltage-gated sodium channel α(I) subunit (Na(v)1.1). We have previously reported that mice heterozygous for a nonsense mutation in Scn1a developed early onset epileptic seizures. However, the learning ability and sociability of the mice remained to be investigated. In the present study, we subjected heterozygous Scn1a mice to a comprehensive behavioral test battery. We found that while heterozygous Scn1a mice had lowered spontaneous motor activity in home cage, they were hyperactive in novel environments. Moreover, the mice had low sociability and poor spatial learning ability that correspond to the autistic behaviors and cognitive decline seen in Dravet syndrome patients. These results suggest that Na(v)1.1 haploinsufficiency intrinsically contributes to not only epileptic seizures but also lowered sociability and learning impairment in heterozygous Scn1a mutant mice, as it should also be the case in patients with Dravet syndrome.
Neurobiol Dis. 2012 Aug 25;49C:211-220. doi: 10.1016/j.nbd.2012.08.012. [Epub ahead of print]
Preferential inactivation of Scn1a in parvalbumin interneurons increases seizure susceptibility.
Dutton SB, Makinson CD, Papale LA, Shankar A, Balakrishnan B, Nakazawa K, Escayg A.
Department of Human Genetics, Emory University, Atlanta, GA, 30022, USA.
Voltage-gated sodium channels (VGSCs) are essential for the generation and propagation of action potentials in electrically excitable cells. Dominant mutations in SCN1A, which encodes the Na(v)1.1 VGSC α-subunit, underlie several forms of epilepsy, including Dravet syndrome (DS) and genetic epilepsy with febrile seizures plus (GEFS+). Electrophysiological analyses of DS and GEFS+ mouse models have led to the hypothesis that SCN1A mutations reduce the excitability of inhibitory cortical and hippocampal interneurons. To more directly examine the relative contribution of inhibitory interneurons and excitatory pyramidal cells to SCN1A-derived epilepsy, we first compared the expression of Na(v)1.1 in inhibitory parvalbumin (PV) interneurons and excitatory neurons from P22 mice using fluorescent immunohistochemistry. In the hippocampus and neocortex, 69% of Na(v)1.1 immunoreactive neurons were also positive for PV. In contrast, 13% and 5% of Na(v)1.1 positive cells in the hippocampus and neocortex, respectively, were found to co-localize with excitatory cells identified by CaMK2α immunoreactivity. Next, we reduced the expression of Scn1a in either a subset of interneurons (mainly PV interneurons) or excitatory cells by crossing mice heterozygous for a floxed Scn1a allele to either the Ppp1r2-Cre or EMX1-Cre transgenic lines, respectively. The inactivation of one Scn1a allele in interneurons of the neocortex and hippocampus was sufficient to reduce thresholds to flurothyl- and hyperthermia-induced seizures, whereas thresholds were unaltered following inactivation in excitatory cells. Reduced interneuron Scn1a expression also resulted in the generation of spontaneous seizures. These findings provide direct evidence for an important role of PV interneurons in the pathogenesis of Scn1a-derived epilepsies.
Nature. 2012 Sep 20;489(7416):385-90. doi: 10.1038/nature11356. Epub 2012 Aug 22.
Autistic-like behaviour in Scn1a+/- mice and rescue by enhanced GABA-mediated neurotransmission.
Han S, Tai C, Westenbroek RE, Yu FH, Cheah CS, Potter GB, Rubenstein JL, Scheuer T, de la Iglesia HO, Catterall WA.
Graduate Program in Neurobiology & Behavior, University of Washington, Seattle, Washington 98195, USA.
Haploinsufficiency of the SCN1A gene encoding voltage-gated sodium channel Na(V)1.1 causes Dravet’s syndrome, a childhood neuropsychiatric disorder including recurrent intractable seizures, cognitive deficit and autism-spectrum behaviours. The neural mechanisms responsible for cognitive deficit and autism-spectrum behaviours in Dravet’s syndrome are poorly understood. Here we report that mice with Scn1a haploinsufficiency exhibit hyperactivity, stereotyped behaviours, social interaction deficits and impaired context-dependent spatial memory. Olfactory sensitivity is retained, but novel food odours and social odours are aversive to Scn1a(+/-) mice. GABAergic neurotransmission is specifically impaired by this mutation, and selective deletion of Na(V)1.1 channels in forebrain interneurons is sufficient to cause these behavioural and cognitive impairments. Remarkably, treatment with low-dose clonazepam, a positive allosteric modulator of GABA(A) receptors, completely rescued the abnormal social behaviours and deficits in fear memory in the mouse model of Dravet’s syndrome, demonstrating that they are caused by impaired GABAergic neurotransmission and not by neuronal damage from recurrent seizures. These results demonstrate a critical role for Na(V)1.1 channels in neuropsychiatric functions and provide a potential therapeutic strategy for cognitive deficit and autism-spectrum behaviours in Dravet’s syndrome.
Proc Natl Acad Sci U S A. 2012 Sep 4;109(36):14646-51. doi: 10.1073/pnas.1211591109. Epub 2012 Aug 20.
Specific deletion of NaV1.1 sodium channels in inhibitory interneurons causes seizures and premature death in a mouse model of Dravet syndrome.
Cheah CS, Yu FH, Westenbroek RE, Kalume FK, Oakley JC, Potter GB, Rubenstein JL, Catterall WA.
Department of Pharmacology, University of Washington, Seattle, WA 98195, USA.
Heterozygous loss-of-function mutations in the brain sodium channel Na(V)1.1 cause Dravet syndrome (DS), a pharmacoresistant infantile-onset epilepsy syndrome with comorbidities of cognitive impairment and premature death. Previous studies using a mouse model of DS revealed reduced sodium currents and impaired excitability in GABAergic interneurons in the hippocampus, leading to the hypothesis that impaired excitability of GABAergic inhibitory neurons is the cause of epilepsy and premature death in DS. However, other classes of GABAergic interneurons are less impaired, so the direct cause of hyperexcitability, epilepsy, and premature death has remained unresolved. We generated a floxed Scn1a mouse line and used the Cre-Lox method driven by an enhancer from the Dlx1,2 locus for conditional deletion of Scn1a in forebrain GABAergic neurons. Immunocytochemical studies demonstrated selective loss of Na(V)1.1 channels in GABAergic interneurons in cerebral cortex and hippocampus. Mice with this deletion died prematurely following generalized tonic-clonic seizures, and they were equally susceptible to thermal induction of seizures as mice with global deletion of Scn1a. Evidently, loss of Na(V)1.1 channels in forebrain GABAergic neurons is both necessary and sufficient to cause epilepsy and premature death in DS.
Therapie. 2012 Mar-Apr;67(2):157-60. doi: 10.2515/therapie/2012014. Epub 2012 Aug 2.
[Therapeutic drug monitoring of stiripentol].
[Article in French]
Verdier MC, Tribut O, Bentué-Ferrer D.
CHU Pontchaillou, Laboratoire de Pharmacologie Biologique, Rennes, France.
Stiripentol is a third generation antiepileptic, marketed since 2007 under the name of Diacomit(®). It is indicated, always in combination, in the treatment of severe myoclonic epilepsy in infancy or Dravet syndrome. Its pharmacokinetics is not linear. It is a potent inhibitor of CYP3A4, 1A2 and 2C19 and increases the plasma concentrations of many other antiepileptic drugs. Without this being considered as a validated therapeutic range, the trough plasma concentrations at steady-state, corresponding to the usual doses are between 10 and 15 mg/L. The concentration-efficacy relationship is not established, but there is some evidence for a concentration-related toxicity. However, because of its non-linear kinetics, stiripentol should be a good candidate for therapeutic drug monitoring (TDM). Nonetheless, the current level of evidence for the advantage of TDM is « remains to be estimated ».
PLoS One. 2012;7(7):e41802. doi: 10.1371/journal.pone.0041802. Epub 2012 Jul 25.
Identification of SCN1A and PCDH19 mutations in Chinese children with Dravet syndrome.
Kwong AK, Fung CW, Chan SY, Wong VC.
Department of Paediatrics and Adolescent Medicine, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong SAR, China.
BACKGROUND:
Dravet syndrome is a severe form of epilepsy. Majority of patients have a mutation in SCN1A gene, which encodes a voltage-gated sodium channel. A recent study has demonstrated that 16% of SCN1A-negative patients have a mutation in PCDH19, the gene encoding protocadherin-19. Mutations in other genes account for only a very small proportion of families. TSPYL4 is a novel candidate gene within the locus 6q16.3-q22.31 identified by linkage study.
OBJECTIVE:
The present study examined the mutations in epileptic Chinese children with emphasis on Dravet syndrome.
METHODS:
A hundred children with severe epilepsy were divided into Dravet syndrome and non-Dravet syndrome groups and screened for SCN1A mutations by direct sequencing. SCN1A-negative Dravet syndrome patients and patients with phenotypes resembling Dravet syndrome were checked for PCDH19 and TSPYL4 mutations.
RESULTS:
Eighteen patients (9 males, 9 females) were diagnosed to have Dravet syndrome. Among them, 83% (15/18) had SCN1A mutations including truncating (7), splice site (2) and missense mutations (6). The truncating/splice site mutations were associated with moderate to severe degree of intellectual disability (p<0.05). During the progression of disease, 73% (11/15) had features fitting into the diagnostic criteria of autism spectrum disorder and 53% (8/15) had history of vaccination-induced seizures. A novel PCDH19 p.D377N mutation was identified in one SCN1A-negative female patient with Dravet syndrome and a known PCDH19 p.N340S mutation in a female non-Dravet syndrome patient. The former also inherited a TSPYL4 p.G60R variant.
CONCLUSION:
A high percentage of SCN1A mutations was identified in our Chinese cohort of Dravet syndrome patients but none in the rest of patients. We demonstrated that truncating/splice site mutations were linked to moderate to severe intellectual disability in these patients. A de novo PCDH19 missense mutation together with an inherited TSPYL4 missense variant were identified in a patient with Dravet syndrome.
Brain. 2012 Aug;135(Pt 8):2309-11. doi: 10.1093/brain/aws198.
How Dravet syndrome became a model for studying childhood genetic epilepsies.
Dravet C.
Childhood Neuropsychiatric Unit, Catholic University, Roma, Italy. charlotte.dravet@free.fr
Comment on
- Prognostic, clinical and demographic features in SCN1A mutation-positive Dravet syndrome. [Brain. 2012]
Prognostic, clinical and demographic features in SCN1A mutation-positive Dravet syndrome.Brunklaus A, Ellis R, Reavey E, Forbes GH, Zuberi SM. Brain. 2012 Aug; 135(Pt 8):2329-36. Epub 2012 Jun 19.
Epilepsy Res. 2013 Jan;103(1):88-96. doi: 10.1016/j.eplepsyres.2012.07.
An electroclinical study of absence seizures in Dravet syndrome.
Tsuda Y, Oguni H, Sakauchi M, Osawa M.
Department of Pediatrics, Tokyo Women’s Medical University, Tokyo, Japan.
We studied clinical and EEG manifestations of absence seizures (AS) in children with Dravet syndrome (DS) to clarify their characteristic features and differences from those of typical AS (TAS). The subjects were 12 children with DS. We retrospectively analyzed electroclinical characteristics of AS. We analyzed a total of 102 ictal EEGs characterized by generalized spike-and-wave (GSW) and semiology of 78 video-taped AS. The mean age at the onset of AS and at the time of the study was 16.2±7.1 months and 40.3±22.1 months, respectively. Ictal EEG showed the focality of initial discharge in 49/102 (48%), a duration ranging from 2 to 180 s (mean: 10.2±22.6 s; median: 4.0 s), frequency ranging from 2 to 4 Hz (median=3.0 Hz), and irregular and disorganized GSW morphology in 66/102 (65%). AS manifested with eyelid-myoclonus and generalized myoclonus in 9/54 (17%) and 34/78 (44%), respectively. In conclusion, AS in DS were characterized by an early-onset age, a high incidence of irregular and disorganized 3 Hz GSW morphology, and the frequent association of generalized myoclonic movement as well as the absence of automatism as compared to TAS. The results should be appreciated in the differential diagnosis of early-onset AS, the treatment of AS in DS and also a further clinical and genetic study for DS.
Epilepsia. 2012 Aug;53(8):1349-59. doi: 10.1111/j.1528-1167.2012.
Investigation of hypoxia-inducible factor-1α in hippocampal sclerosis: a postmortem study.
Feast A, Martinian L, Liu J, Catarino CB, Thom M, Sisodiya SM.
Departments of Clinical and Experimental Epilepsy Neuropathology Neurology, UCL, Institute of Neurology, Queen Square, London, United Kingdom.
PURPOSE:
Hypoxia-inducible factor-1α (HIF-1α) is involved in critical aspects of cell survival in response to hypoxia and regulates vascular endothelial growth factor (VEGF) expression. Previous experimental and human studies in epilepsy show up-regulation of VEGF following seizures, although expression of HIF-1α as its potential regulator has not been explored. We used a postmortem (PM) series from patients with epilepsy and hippocampal sclerosis (HS) to investigate patterns of expression of HIF-1α and VEGF and their potential contribution to neuroprotection.
METHOD:
In 33 PMs (17 cases with unilateral HS, 3 with bilateral HS, 3 with No-HS, and 10 controls), we quantified neuronal immunolabeling for HIF-1α and VEGF in hippocampal subfields.
KEY FINDINGS:
HIF-1α- and VEGF-immunopositive hippocampal neurones were observed in HS, No-HS, and also in control cases; there was no significant difference in overall labeling between epilepsy cases and controls. In positive cases, HIF-1α and VEGF neuronal labeling localized primarily in CA1, CA4, and CA3 subfields in all groups; significantly more positive neurons were seen in the entorhinal cortex in epilepsy cases (p < 0.05). Labeling lateralized to the side of sclerosis in unilateral HS cases, with significant differences between hemispheres (p < 0.05). There was a trend for high HIF-1α labeling scores in patients with Dravet syndrome without HS and sudden unexpected death in epilepsy (SUDEP) cases, and lower scores with long seizure-free periods prior to death. Hippocampal HIF-1α and VEGF labeling showed a significant correlation. There was neuronal colocalization of HIF-1α and VEGF.
SIGNIFICANCE:
Regional expression patterns are in keeping with seizure-related activation of HIF-1α and VEGF. The prominent expression in non-HS cases could support an overall neuroprotective effect. Correlation between HIF-1α and VEGF neuronal immunolabeling supports HIF-1α-mediated induction of VEGF in epilepsy.
Sodium Channel Mutations and Epilepsy [Internet].
Catterall WA.
In: Noebels JL, Avoli M, Rogawski MA, Olsen RW, Delgado-Escueta AV, editors.
Jasper’s Basic Mechanisms of the Epilepsies [Internet]. 4th edition. Bethesda (MD): National Center for Biotechnology Information (US); 2012.
Excerpt
Voltage-gated sodium channels initiate action potentials in brain neurons, and sodium channel blockers are used in therapy of epilepsy. Mutations in sodium channels are responsible for genetic epilepsy syndromes with a wide range of severity. Generalized Epilepsy with Febrile Seizures Plus (GEFS+) is caused by missense mutations in NaV1.1 channels, which have variable functional effects on sodium channels expressed in non-neuronal cells, but may primarily cause loss of function when expressed in mice. Complete loss-of-function mutations in NaV1.1 cause Severe Myoclonic Epilepsy of Infancy (SMEI or Dravet Syndrome), which involves severe, intractable epilepsy and co-morbidities of ataxia, sleep disturbance, and cognitive impairment. Mice with loss-of-function mutations in NaV1.1 channels have severely impaired sodium currents and action potential firing in hippocampal GABAergic inhibitory neurons without detectable effect on the excitatory pyramidal neurons, which would cause hyperexcitability and contribute to seizures in SMEI. Similarly, sodium currents and action potential firing are impaired in the GABAergic Purkinje neurons in the cerebellum, which likely contributes to ataxia, and in the reticular nucleus of the thalamus and the suprachiasmatic nucleus of the hypothalamus, which likely contribute to circadian rhythm disturbances and sleep disorder. The imbalance between excitatory and inhibitory transmission can be partially corrected by compensatory loss-of-function mutations of NaV1.6 channels, and thermally induced seizures in these mice can be prevented by drug combinations that enhance GABAergic neurotransmission. Familial Febrile Seizures are also caused by mild loss-of-function mutations in NaV1.1 channels. We have proposed a unified loss-of-function hypothesis for the spectrum of epilepsy syndromes caused by genetic changes in NaV1.1 channels: mild impairment predisposes to febrile seizures, intermediate impairment leads to GEFS+ epilepsy, and severe loss of function causes the intractable seizures and co-morbidities of SMEI. Surprisingly, mutations in other sodium channels that cause epilepsy are rare, but Benign Neonatal Infantile Seizures is caused by mutations in NaV1.2 channels, and mutations in those channels can also lead to more severe epilepsy syndromes. Understanding the molecular and cellular mechanisms that underlie these genetic epilepsies is yielding much information about non-genetic epilepsy syndromes as well.
Genes in infantile epileptic encephalopathies [Internet].
Depienne C, Gourfinkel-An I, Baulac S, LeGuern E.
In: Noebels JL, Avoli M, Rogawski MA, Olsen RW, Delgado-Escueta AV, editors.
Jasper’s Basic Mechanisms of the Epilepsies [Internet]. 4th edition. Bethesda (MD): National Center for Biotechnology Information (US); 2012.
Excerpt
Infantile epileptic encephalopathies, such as Dravet syndrome, Ohtahara syndrome, West syndrome, Lennox-Gastaut syndrome, myoclonic-astatic epilepsy, and Landau-Kleffner syndrome, are devastating epilepsies. Cases are often sporadic or patients have only a limited family history of epilepsy. Although a complex inheritance has long been suspected in epilepsy, recent data indicate that many sporadic rare epileptic disorders, such as Dravet syndrome, CDKL5/STK9 Rett-like epileptic encephalopathy, ARX-related epilepsies, SRPX2-related rolandic epilepsy associated with oral and speech dyspraxia and mental retardation, andSTXBP1-related West/Ohtahara syndromes, are due to a mutation in a unique gene. Dravet syndrome, for example, is mainly due to de novo mutations in SCN1A, the gene encoding the voltage-gated neuronal sodium channel alpha 1 subunit, which explains why most patients are isolated cases. All types of mutations are observed: missense mutations, premature termination codon and intragenic rearrangements. This large mutation spectrum contrasts with that of generalized epilepsy with febrile seizures plus (GEFS+), an autosomal dominant condition also characterized by febrile and afebrile seizures but with a usually benign outcome, in which only missense mutations are found. Recently, mutations in PCDH19, encoding protocadherin 19 on chromosome X, were identified in females with an EFMR or Dravet-like phenotype. Heterozygous females are affected while hemizygous males are spared, this unusual inheritance probably being due to a mechanism called cellular interference. The genetic data accumulated for Dravet syndrome and other related disorders have to be kept in mind when studying epileptic encephalopathies.
GABAA Receptor Subunit Mutations and Genetic Epilepsies [Internet].
Macdonald RL, Kang JQ, Gallagher MJ.
In: Noebels JL, Avoli M, Rogawski MA, Olsen RW, Delgado-Escueta AV, editors.
Jasper’s Basic Mechanisms of the Epilepsies [Internet]. 4th edition. Bethesda (MD): National Center for Biotechnology Information (US); 2012.
Excerpt
Mutations in inhibitory GABAA receptor subunit genes (GABRA1, GABRB3, GABRG2 and GABRD) have been associated with idiopathic epilepsy syndromes (IES) including childhood absence epilepsy (CAE), juvenile myoclonic epilepsy (JME), pure febrile seizures (FS), generalized epilepsy with febrile seizures plus (GEFS+), and Dravet syndrome (DS) (also known as severe myoclonic epilepsy in infancy, SMEI). These mutations are found in both translated and untranslated gene regions and have been shown to affect the GABAA receptors by altering receptor function and/or by impairing receptor biogenesis by multiple mechanisms including reducing subunit mRNA transcription or stability, impairing subunit folding, stability, or oligomerization or by inhibiting receptor trafficking. While a clear genotype/phenotype correlation has not been established, mutations of GABRB3 and GABRA1are associated with CAE or JME while mutations and variants of GABRG2 and GABRD are associated with FS, FS with CAE, GEFS+, and DS.
Epilepsia. 2012 Aug;53(8):1421-8. doi: 10.1111/j.1528-1167.2012.
Dravet syndrome: seizure control and gait in adults with different SCN1A mutations.
Rilstone JJ, Coelho FM, Minassian BA, Andrade DM.
Program in Genetics and Genomic Biology, The Hospital for Sick Children, Toronto, Ontario, Canada.
PURPOSE:
Dravet syndrome (DS) is an aggressive epileptic encephalopathy. Pharmacoresistant seizures of several types plague most patients with DS throughout their lives. Gait difficulties are a common, but inconsistent finding. The majority of cases are caused by mutations in the SCN1A gene, but little information is available about how particular mutations influence the adult phenotype. The purpose of this study is to correlate different types of SCN1A mutations and (1) seizure control, (2) occurrence of convulsive status epilepticus (cSE), and (3) the presence of crouch gait in adult patients.
METHODS:
In a cohort of 10 adult patients with DS caused by SCN1A mutations, we investigated seizure frequency, history of cSE, and gait. All patients were identified in the epilepsy clinic between 2009 and 2011. SCN1A mutations were divided into four different groups based on location or effect of the mutation. Retrospective chart review and recent physical examination were completed in all cases.
KEY FINDINGS:
All patients had a pathogenic mutation in the SCN1A gene. Four SCN1A mutations have not been described previously. Greater than 90% seizure reduction was observed (compared to childhood frequency) in six of seven patients with missense mutations in the pore-forming region (PFR) of the Na(v) 1.1 protein (group A) and nonsense mutations (group B). One patient with a splice-site mutation (group C) and another with a mutation outside the PFR (group D) became free of all types of seizures. cSE after the age of 19 years was observed in only one patient. Crouch gait, without spasticity, is identified as an element of the adult DS phenotype. However, only one half of our adult DS cohort demonstrated crouch gait. This feature was observed in five of seven patients from groups A and B.
SIGNIFICANCE:
This study shows that seizure control improves and cSE become less frequent in DS as patients age, independent of their SCN1A mutation type. Complete seizure freedom was seen in two patients (groups C and D). Finally, this study shows that in DS, crouch gait can be observed in up to 50% of adults with SCN1A mutation. Although no definite statistical correlations could be made due to the small number of patients, it is interesting to note that crouch gait was observed only in those patients with nonsense mutations or mutations in the PFR. Future studies with larger cohorts will be required to formally assess an association of gait abnormalities with particular SCN1A mutations.
Neurobiol Dis. 2012 Oct;48(1):115-23. doi: 10.1016/j.nbd.2012.06.013. Epub 2012 Jun 30.
The GABRG2 nonsense mutation, Q40X, associated with Dravet syndrome activated NMD and generated a truncated subunit that was partially rescued by aminoglycoside-induced stop codon read-through.
Huang X, Tian M, Hernandez CC, Hu N, Macdonald RL.
The Graduate Program of Neuroscience, Vanderbilt University Medical Center, Nashville, TN 37212, USA.
The GABRG2 nonsense mutation, Q40X, is associated with the severe epilepsy syndrome, Dravet syndrome, and is predicted to generate a premature translation-termination codon (PTC) in the GABA(A) receptor γ2 subunit mRNA in a position that codes for the first amino acid of the mutant subunit. We determined the effects of the mutation on γ2 subunit mRNA and protein synthesis and degradation, as well as on α1β2γ2 GABA(A) receptor assembly, trafficking and surface expression in HEK cells. Using bacterial artificial chromosome (BAC) constructs, we found that γ2(Q40X) subunit mRNA was degraded by nonsense mediated mRNA decay (NMD). Undegraded mutant mRNA was translated to a truncated peptide, likely the signal peptide, which was cleaved further. We also found that mutant γ2(Q40X) subunits did not assemble into functional receptors, thus decreasing GABA-evoked current amplitudes. The GABRG2(Q40X) mutation is one of several epilepsy-associated nonsense mutations that have the potential to be rescued by reading through the PTC, thus restoring full-length protein translation. As a first approach, we investigated the use of the aminoglycoside, gentamicin, to rescue translation of intact mutant subunits by inducing mRNA read-through. In the presence of gentamicin, synthesis of full length γ2 subunits was partially restored, and surface biotinylation and whole cell recording experiments suggested that rescued γ2 subunits could corporate into functional, surface GABA(A) receptors, indicating a possible direction for future therapy.
Ther Drug Monit. 2012 Aug;34(4):390-7. doi: 10.1097/FTD.0b013e31825dc4a6.
Concentrations of stiripentol in children and adults with epilepsy: the influence of dose, age, and comedication.
May TW, Boor R, Mayer T, Jürgens U, Rambeck B, Holert N, Korn-Merker E, Brandt C.
Pharmacological Laboratory, Society for Epilepsy Research, Bielefeld, Germany. Theodor.May@evkb.de
BACKGROUND:
Stiripentol (STP) was approved as an orphan drug in 2007 in Europe as adjunctive therapy with valproic acid (VPA) and clobazam (CLB) for Dravet syndrome. Dravet syndrome is a highly pharmacoresistant form of epilepsy, which starts in early childhood. Data about STP pharmacokinetics and interactions are still limited and in part inconsistent. The aim of our study was to analyze the effect of age, gender, daily STP dose per body weight (milligrams per kilogram), VPA, CLB, and enzyme-inducing antiepileptic drugs on STP concentration-to-dose ratio (CDR), STP clearance, and STP trough concentrations.
METHODS:
Retrospectively, 220 STP serum concentrations in 75 patients from 3 German Epilepsy Centers were analyzed. Analysis of variance, regression analysis, and generalized estimating equations were used for statistical analysis.
RESULTS:
Our findings confirm the nonlinear STP pharmacokinetics. At steady state, STP CDR increased with daily STP doses. Compared with patients older than 12 years, STP concentrations were decreased by 39.6% in children aged 6-12 years (P < 0.001) and by 57.5% in children younger than 6 years (P < 0.001). Phenobarbital and phenytoin decreased STP concentrations by 63.2%. This effect was highly significant (P < 0.001), despite the small number of patients (n = 7) treated with phenobarbital or phenytoin. VPA had no significant effect on STP serum concentrations, whereas STP serum concentrations were moderately but significantly increased by CLB (24.6%, P = 0.011).
CONCLUSIONS:
Therapeutic drug monitoring of STP seems to be useful because of the wide variation of STP CDR, the nonlinear concentration-to-dose relationship, age-dependent pharmacokinetics, and drug-drug interactions.
Brain. 2012 Aug;135(Pt 8):2329-36. doi: 10.1093/brain/aws151. Epub 2012 Jun 19.
Prognostic, clinical and demographic features in SCN1A mutation-positive Dravet syndrome.
Brunklaus A, Ellis R, Reavey E, Forbes GH, Zuberi SM.
The Paediatric Neurosciences Research Group, Royal Hospital for Sick Children, Yorkhill, Dalnair Street, Glasgow G3 8SJ, UK.
Comment in
- How Dravet syndrome became a model for studying childhood genetic epilepsies. [Brain. 2012]
How Dravet syndrome became a model for studying childhood genetic epilepsies.Dravet C. Brain. 2012 Aug; 135(Pt 8):2309-11.
Dravet syndrome is a severe infantile onset epileptic encephalopathy associated with mutations in the sodium channel alpha 1 subunit gene SCN1A. To date no large studies have systematically examined the prognostic, clinical and demographic features of the disease. We prospectively collected data on a UK cohort of individuals with Dravet syndrome during a 5-year study period and analysed demographic information based on UK population and birth figures. From structured referral data we examined a range of clinical characteristics including epilepsy phenotype, seizure precipitants, electroencephalography data, imaging studies, mutation class and response to medication. Predictors of developmental outcome were determined by logistic regression. We identified 241 cases with SCN1A mutation-positive Dravet syndrome, 207 of which were UK-based. The incidence of mutation-positive Dravet syndrome is at least 1:40 900 UK births. Clinical features predicting a worse developmental outcome included status epilepticus (odds ratio = 3.1; confidence interval = 1.5-6.3; P = 0.003), interictal electroencephalography abnormalities in the first year of life (odds ratio = 5.7; confidence interval = 1.9-16.8; P = 0.002) and motor disorder (odds ratio = 3.3; confidence interval = 1.7-6.4; P < 0.001). No significant effect was seen for seizure precipitants, magnetic resonance imaging abnormalities or mutation class (truncating versus missense). Abnormal magnetic resonance imaging was documented in 11% of cases, principally with findings of non-specific brain atrophy or hippocampal changes. Sodium valproate, benzodiazepines and topiramate were reported as being the most helpful medications at the time of referral. Aggravation of seizures was reported for carbamazepine and lamotrigine. The identification of factors influencing prognosis both aids counselling and encourages early, syndrome-specific therapy. Prevention of status epilepticus with regular medication and emergency protocols is important and may influence developmental outcome.
Eur J Paediatr Neurol. 2012 Sep;16 Suppl 1:S1-4. doi: 10.1016/j.ejpn.2012.04.006. Epub 2012 Jun 15.
Dravet syndrome: the main issues.
Guerrini R.
Pediatric Neurology and Neurogenetics Unit and Laboratories, Children’s Hospital A Meyer, University of Florence, Firenze, Italy.r.guerrini@meyer.it
Dravet syndrome (DS) is a severe form of infantile onset epilepsy characterized by multiple seizure types, prolonged convulsive seizures and frequent episodes of status epilepticus. Seizures precipitated by fever are a main characteristic. Affected children exhibit normal early development. Cognitive impairment, behavioral disturbances with hyperactivity and sometimes autistic traits occur after seizure onset. Seizures persist into adulthood but become less frequent. In about 85% of patients, a mutation of the SCN1A gene is present. DS fully illustrates the concept of epileptic encephalopathy. However, it is difficult to determine the causative role of the underlying sodium channel dysfunction and that of the consequent seizures in influencing cognitive outcome. An overwhelmingly high number of SCN1A mutations have been associated with DS. Intragenic or whole gene deletions, duplications and amplifications are additional rare molecular mechanisms. Most mutations are de novo, but familial mutations also occur. Somatic mosaic mutations should be considered when estimating the recurrence. MRI imaging is usually normal, and no neuropathologic signature of the condition seems to exist. In heterozygous Scn1a+/- mice, GABAergic interneurons exhibit substantially reduced sodium current density with reduced ability for sustained action potential firing. GABAergic output is reduced and excitability of downstream synaptic targets increased. Stiripentol was effective in combination with valproate and clobazam in two pivotal phase III trials. Phenytoin, carbamazepine, and lamotrigine can worsen seizures and should be avoided. Prospective studies will clarify to what extent earlier diagnosis and efforts at seizure control with the most appropriate drug combinations will reduce clinical deterioration.
Eur J Paediatr Neurol. 2012 Sep;16 Suppl 1:S5-8. doi: 10.1016/j.ejpn.2012.04.007. Epub 2012 Jun 16.
Diagnosis and long-term course of Dravet syndrome.
Scheffer IE.
Department of Medicine and Paediatrics, Florey Neuroscience Institutes, University of Melbourne, Austin Health and Royal Children’s Hospital, Melbourne, Australia. scheffer@unimelb.edu.au
Dravet syndrome is a severe infantile-onset epilepsy syndrome with a distinctive but complex electroclinical presentation. A healthy, developmentally normal infant presents at around 6 months of age with convulsive status epilepticus, which may be hemiclonic or generalized; seizures may be triggered by fever, illness or vaccination. The infant typically has further episodes of status epilepticus every month or two, often triggered by fever. Other seizure types including focal dyscognitive seizures, absence and myoclonic seizures develop between 1 and 4 years. Atonic drop attacks and episodes of non-convulsive status may occur. Early development is normal but slows in the second year. Developmental regression may occur, particularly with status epilepticus. EEG studies are initially normal, but after 2 years they show generalized spike-wave and polyspike-wave activity with multifocal discharges. Photosensitivity may be seen. Imaging is normal or shows non-specific findings such as atrophy. Dravet syndrome is associated with mutations of the gene encoding the alpha-1 subunit of the sodium channel, SCN1A, in >70% of patients. These include sequencing mutations and copy number variant anomalies; 90% of mutations arise de novo. PCDH19 mutational analysis is a second-tier test for girls with a Dravet-like picture who do not have SCN1A mutations. Outcome is poor, with intellectual disability in most patients and ongoing seizures. Intellectual impairment varies from severe in 50% patients, to moderate and mild intellectual disability each accounting for 25% cases. Rare patients have normal intellect. The long-term course involves ongoing, brief nocturnal convulsions and a characteristic deterioration in gait.
Eur J Paediatr Neurol. 2012 Sep;16 Suppl 1:S13-7. doi: 10.1016/j.ejpn.2012.04.009. Epub 2012 Jun 12.
Stiripentol: an example of antiepileptic drug development in childhood epilepsies.
Nabbout R, Chiron C.
Department of Pediatric Neurology, Centre de Reference des Epilepsies Rares, Inserm U663, Hopital Necker Enfants Malades, APHP, Paris Descartes University, Paris, France. rimanabbout@yahoo.com
The efficacy of stiripentol (STP) in Dravet Syndrome (DS) was discovered first in an exploratory study in pediatric pharmacoresistant epilepsies. This efficacy signal, used as a proof of concept, led to – two independent multicenter randomized, double-blind, placebo-controlled trials in DS patients: STICLO-France and STICLO-Italy. In adjunction to valproate and clobazam, STP demonstrated marked efficacy and these trials became the basis for the registration of STP as an orphan drug for DS. Although STP had previously shown antiepileptic activity, since it inhibits cytochromes P450, the increased plasma levels of clobazam (CLB), norclobazam (NCLB), and NCLB/CLB ratio reported in STICLO studies brought into question the activity of STP per se. Recent pharmacological studies demonstrated that (i) STP is a direct allosteric modulator of the GABA receptors at a site distinct from benzodiazepines; (ii) STP and CLB/NCLB act independently at GABA(A) receptors; (iii) their combination increases the maximum response beyond that of either drug alone. All these effects are independent of considerations of changes in metabolism. Some responders in STICLO studies failed to display any increase of plasmatic concentrations of NCLB/CLB ratio as STP could not inhibit CYP2C19 because of its inhibition by progabide or due to an inactivating CYP polymorphism. The responder rate proved to be in the same range whether the NCLB/CLB ratio increased or not. These analyses confirmed that the effects of STP cannot result from a simple pharmacokinetic interaction. We propose that the success of STP should serve as a model for AED development in rare pediatric epileptic syndromes.
Eur J Paediatr Neurol. 2012 Sep;16 Suppl 1:S18-20. doi: 10.1016/j.ejpn.2012.04.010. Epub 2012 Jun 12.
Addressing the needs of patients and their family: conclusion.
Dravet C.
Centre Saint-Paul-Hôpital Henri Gastaut, Marseille, France. charlotte.dravet@free.fr
Four steps, which have been clearly described in the previous texts, can be used to help families of patients with Dravet syndrome. The first is the right diagnosis. The article by I. Scheffer reviewed the clinical presentation of Dravet syndrome. Diagnosis at the onset is sometimes difficult. In doubtful cases, when convulsive seizures are repeated and prolonged, I advocate early treatment under the presumption that it may be Dravet syndrome, so that complications such as status epilepticus or inappropriate use of antiepileptic drugs may be avoided. The occurrence of photosensitivity is difficult to quantify because it is variable and is dependent on the inclusion or exclusion of pattern-sensitivity and eye closure effect. Differences may exist between countries, but in our experience it is much more frequent than 10% of cases. The second step is use of the appropriate treatment. As shown by R. Nabbout, the development of stiripentol provided great progress in treatment, since it is the only drug that has demonstrated efficacy in double-blind clinical studies. I hope ongoing studies will lead to its wider use in more patients and that other new drugs will be developed. The third step is addressing the burden of the disease on the families. P. Camfield, in his presentation of family problems, has considered this aspect in a realistic way. In the most severe patients, the placement of an indwelling catheter is undoubtedly a means of preventing status epilepticus. The designation of one parent to be « on call » for the affected child and the other for the siblings is another good suggestion. The fourth step is understanding the factors responsible for the cognitive decline, which were explained by R. Guerrini, and providing the families with all possible assistance in order to decrease this risk. The distribution of cognitive levels depends on the time when patients were evaluated. Update data tend to indicate that those recently diagnosed appear to have less severe decline than those diagnosed long ago, perhaps as a result of better patient management.
Eur J Paediatr Neurol. 2012 Sep;16 Suppl 1:S9-12. doi: 10.1016/j.ejpn.2012.04.008. Epub 2012 Jun 12.
Helping families cope with the devastation of Dravet syndrome.
Camfield P, Camfield C, Nolan K.
Department of Paediatrics, Dalhousie University and the IWK Health Centre, Halifax, Nova Scotia, Canada. Camfield@dal.ca
Dravet syndrome shakes family life to the core. Seizure control is rarely complete, and simply prescribing medication is inadequate to help families. Our suggestions are based on structured interviews with >25 Dravet families. In Stage 1 (up to 1-1½ years), a written protocol for an organized approach to status epilepticus is mandatory. In Stage 2 (age from 1½ to ~6-10 years), assistance in finding qualified baby sitters (extended family and others) is required. Equipment, rescue medication and protocols should accompany the child. Siblings may benefit from assigning one parent to be « on call », and an Internet support group provides an invaluable lifeline. In Stage 3 (after ~10 years), family isolation may become extreme: respite care and personal time for parents are important. An epilepsy transition clinic that can effectively liaise with adult emergency services is optimal. Attention to these realities may improve the quality of life for the child and family.
Neurobiol Dis. 2012 Sep;47(3):378-84. doi: 10.1016/j.nbd.2012.05.017. Epub 2012 Jun 4.
Compromised function in the Na(v)1.2 Dravet syndrome mutation R1312T.
Lossin C, Shi X, Rogawski MA, Hirose S.
Department of Neurology, School of Medicine, University of California-Davis, CA, USA. lossinc@gmail.com
Ion channels, specifically voltage-gated sodium channels (Na(v)s), are common culprits in inheritable seizure disorders. Some Na(v) isoforms are particularly susceptible, while others are only weakly associated with neuronal hyperexcitability. Representative of the latter group is Na(v)1.2 (gene name SCN2A): despite its abundance in the brain, Na(v)1.2-related epilepsy is rare and only few studies have been conducted as to the pathophysiological basis of Na(v)1.2 in neuronal hyperexcitability. We here present a detailed functional analysis of Na(v)1.2 mutant, R1312T, which was originally found in a child with Dravet syndrome (formerly known as severe myoclonic epilepsy of infancy or SMEI). Whole-cell voltage clamp analysis revealed clearly compromised function: the mutant channels fast- and slow-inactivated at markedly more negative potentials and recovered from fast inactivation more slowly, which resulted in a use-dependent current reduction to less than 50% of wildtype levels. We also noted a small hyperpolarizing shift in the voltage dependence of activation. Our findings expand the spectrum of abnormal Na(v) channel behavior in epilepsy and raise the question as to how loss-of-function in a sodium channel predominantly expressed in excitatory neurons can lead to hyperexcitability.
Hong Kong Med J. 2012 Jun;18(3):263.
Management of Dravet syndrome: emerging clinical insights.
Kapoor S.
Comment on
- Genetic diagnosis of severe myoclonic epilepsy of infancy (Dravet syndrome) with SCN1A mutations in the Hong Kong Chinese patients. [Hong Kong Med J. 2011]
Genetic diagnosis of severe myoclonic epilepsy of infancy (Dravet syndrome) with SCN1A mutations in the Hong Kong Chinese patients.Mak CM, Chan KY, Yau EK, Chen SP, Siu WK, Law CY, Lam CW, Chan AY. Hong Kong Med J. 2011 Dec; 17(6):500-2.
Curr Neurol Neurosci Rep. 2012 Aug;12(4):445-55. doi: 10.1007/s11910-012-0281-8.
Genetics of epilepsy and relevance to current practice.
Michelucci R, Pasini E, Riguzzi P, Volpi L, Dazzo E, Nobile C.
Unit of Neurology, IRCCS Institute of Neurological Sciences, Bellaria Hospital, Via Altura 3, 40139, Bologna, Italy.roberto.michelucci@ausl.bo.it
Genetic factors are likely to play a major role in many epileptic conditions, spanning from classical idiopathic (genetic) generalized epilepsies to epileptic encephalopathies and focal epilepsies. In this review we describe the genetic advances in progressive myoclonus epilepsies, which are strictly monogenic disorders, genetic generalized epilepsies, mostly exhibiting complex genetic inheritance, and SCN1A-related phenotypes, namely genetic generalized epilepsy with febrile seizure plus and Dravet syndrome. Particular attention is devoted to a form of familial focal epilepsies, autosomal-dominant lateral temporal epilepsy, which is a model of non-ion genetic epilepsies. This condition is associated with mutations of the LGI1 gene, whose protein is secreted from the neurons and exerts its action on a number of targets, influencing cortical development and neuronal maturation.
Epilepsia. 2012 Aug;53(8):1387-98. doi: 10.1111/j.1528-1167.2012.
Targeted next generation sequencing as a diagnostic tool in epileptic disorders.
Lemke JR, Riesch E, Scheurenbrand T, Schubach M, Wilhelm C, Steiner I, Hansen J, Courage C, Gallati S, Bürki S, Strozzi S,Simonetti BG, Grunt S, Steinlin M, Alber M, Wolff M, Klopstock T, Prott EC, Lorenz R, Spaich C, Rona S, Lakshminarasimhan M,Kröll J, Dorn T, Krämer G, Synofzik M, Becker F, Weber YG, Lerche H, Böhm D, Biskup S.
Division of Human Genetics, University Children’s Hospital Inselspital, Bern, Switzerland. johannes.lemke@insel.ch
PURPOSE:
Epilepsies have a highly heterogeneous background with a strong genetic contribution. The variety of unspecific and overlapping syndromic and nonsyndromic phenotypes often hampers a clear clinical diagnosis and prevents straightforward genetic testing. Knowing the genetic basis of a patient’s epilepsy can be valuable not only for diagnosis but also for guiding treatment and estimating recurrence risks.
METHODS:
To overcome these diagnostic restrictions, we composed a panel of genes for Next Generation Sequencing containing the most relevant epilepsy genes and covering the most relevant epilepsy phenotypes known so far. With this method, 265 genes were analyzed per patient in a single step. We evaluated this panel on a pilot cohort of 33 index patients with concise epilepsy phenotypes or with a severe but unspecific seizure disorder covering both sporadic and familial cases.
KEY FINDINGS:
We identified presumed disease-causing mutations in 16 of 33 patients comprising sequence alterations in frequently as well as in less commonly affected genes. The detected aberrations encompassed known and unknown point mutations (SCN1A p.R222X, p. E289V, p.379R, p.R393H; SCN2A p.V208E; STXBP1 p.R122X; KCNJ10 p.L68P, p.I129V; KCTD7 p.L108M; KCNQ3 p.P574S; ARHGEF9 p.R290H; SMS p.F58L; TPP1 p.Q278R, p.Q422H; MFSD8 p.T294K), a putative splice site mutation (SCN1A c.693A> p.T/P231P) and small deletions (SCN1A p.F1330Lfs3X [1 bp]; MFSD8 p.A138Dfs10X [7 bp]). All mutations have been confirmed by conventional Sanger sequencing and, where possible, validated by parental testing and segregation analysis. In three patients with either Dravet syndrome or myoclonic epilepsy, we detected SCN1A mutations (p.R222X, p.P231P, p.R393H), even though other laboratories had previously excluded aberrations of this gene by Sanger sequencing or high-resolution melting analysis.
SIGNIFICANCE:
We have developed a fast and cost-efficient diagnostic screening method to analyze the genetic basis of epilepsies. We were able to detect mutations in patients with clear and with unspecific epilepsy phenotypes, to uncover the genetic basis of many so far unresolved cases with epilepsy including mutation detection in cases in which previous conventional methods yielded falsely negative results. Our approach thus proved to be a powerful diagnostic tool that may contribute to collecting information on both common and unknown epileptic disorders and in delineating associated phenotypes of less frequently mutated genes.
Epilepsia. 2012 Jul;53(7):1140-5. doi: 10.1111/j.1528-1167.2012.
Efficacy of stiripentol in hyperthermia-induced seizures in a mouse model of Dravet syndrome.
Cao D, Ohtani H, Ogiwara I, Ohtani S, Takahashi Y, Yamakawa K, Inoue Y.
National Epilepsy Center, Shizuoka Institute of Epilepsy and Neurological Disorders, Shizuoka, Japan.
PURPOSE:
We previously reported a mutant mouse carrying a severe myoclonic epilepsy in infancy (SMEI) mutation in Scn1a. In this study, we examined the susceptibility to hyperthermia-induced seizures of heterozygous Scn1a mutant mice (Scn1a(RX/+)) and wild-type (Scn1a(+/+) ) mice. Then we assessed the efficacy of stiripentol (STP) monotherapy versus STP and clobazam (CLB) combination therapy to prevent hyperthermia-induced seizures in Scn1a(RX/+) mice.
METHODS:
The seizure-inducing body temperatures in Scn1a(RX/+) mice and age-matched Scn1a(+/+) mice were compared in three age groups (1 month, 3-5 months, > 6 months). Then STP, CLB, or STP + CLB was administered intraperitoneally to Scn1a(RX/+) mice of two age groups (p1M, aged 1 month; p5M, aged 5-10 months). The efficacy of medications was assessed by comparing the seizure-inducing body temperature and the duration of seizures.
KEY FINDINGS:
The seizure-inducing body temperature was significantly lower in Scn1a(RX/+) than in Scn1a(+/+) mice for all age groups (p < 0.01). The seizure-inducing body temperature was significantly elevated after administration of STP in p1M (p < 0.05) but not in p5M (p > 0.05), and it was significantly elevated after administration of CLB in both age groups (p < 0.05). The seizure-inducing body temperature was significantly higher after administration of STP + CLB than after administration of CLB in p5M (p < 0.05).
SIGNIFICANCE:
Scn1a (RX/+) mice have increased susceptibility to hyperthermia-induced seizure in all age groups. STP monotherapy is effective in preventing hyperthermia-induced seizures in Scn1a(RX/+) mice aged 1 month, but not in those aged 5 months and older. When used in combination therapy with CLB, STP inhibits the metabolism of CLB and probably synergistically enhances the anticonvulsant effect in mice aged 1 month.
Epilepsy Res. 2012 Jul;100(3):338-43. doi: 10.1016/j.eplepsyres.2011.09.
A parent’s perspective on dietary treatments for epilepsy.
Williams E, Abrahams J, Maguire A, Harris G.
Matthew’s Friends, Dietary Treatments for Epilepsy, GLOBAL, UK. emma@matthewsfriends.org
Four families gave their accounts of the how Dietary Therapies had impacted on their lives and that of their children who suffered with intractable epilepsy. All with very different stories, experiences and outcomes. Niamh was diagnosed with migrating partial epilepsy of infancy with an underlying metabolic problem was fed via her jejunostomy and the parents overcame every obstacle in their path to have as much time with their daughter as possible. Niamh’s family now work with the Matthew’s Friends organization to promote dietary awareness and make these treatments available for all those who need them. Carson, who with infantile spasms, was able to access the diet as her first line treatment without any medication being taken. Carson is the inspiration behind the Carson Harris Foundation and her family promote dietary awareness in USA. Matthew, with Dravet Syndrome, was refused for the diet for years, suffered brain damage and was put on a whole host of unsuitable medications before finally managing to get the diet. The diet proved his saving but what could have been the outcome if the family had got the diet when it was first asked for? Matthew is the inspiration behind the Matthew’s Friends – Dietary Treatments for Epilepsy organization. Charlie, suffered with intractable epilepsy, was put on a whole host of medications that did not work and underwent brain surgery before finally getting to the diet that cured him of his epilepsy. He is the inspiration behind The Charlie Foundation in the USA and his father, Jim Abrahams made the film ‘First Do No Harm’ which told the true story of a child who was cured of his epilepsy using the Ketogenic Diet, just like Charlie and thousands upon thousands of other children around the world. The Charlie Foundation and Matthew’s Friends work side by side in the promotion, education and funding of these treatments and have asked other family organizations to work with them so that families of the future will not have to struggle to gain the information that they so desperately need. Families have the right to make an informed choice and these organizations work together in order to be able to provide this.
Epilepsia. 2012 Jul;53(7):1131-9. doi: 10.1111/j.1528-1167.2012.
Successful use of fenfluramine as an add-on treatment for Dravet syndrome.
Ceulemans B, Boel M, Leyssens K, Van Rossem C, Neels P, Jorens PG, Lagae L.
Department of Neurology-Pediatric Neurology, Antwerp University Hospital, University of Antwerp, Edegem, Belgium.berten.ceulemans@uza.be
PURPOSE:
Despite the development of new antiepileptic drugs, Dravet syndrome frequently remains therapy resistant and is a catastrophic epilepsy syndrome. Fenfluramine is an amphetamine-like drug that has been used in the past as a part of antiobesity treatments. Because of the possible cardiac adverse effects (valve thickening, pulmonary hypertension) associated with use of fenfluramine, it was withdrawn from the market in 2001. In Belgium, a Royal Decree permitted examination of the potential anticonvulsive effects of fenfluramine in a clinical trial consisting of a small group of patients diagnosed with Dravet syndrome.
METHODS:
Herein, we report 12 patients, 7 female and 5 male, with a genetically proven (11 of 12) diagnosis of Dravet syndrome who received fenfluramine as add-on therapy.
KEY FINDINGS:
Their ages at their last evaluation ranged from 3-35 years. The mean dosage of fenfluramine was 0.34 (0.12-0.90) mg/kg/day. Exposure duration to fenfluramine ranged from 1-19 years. Seven of the patients who were still receiving the fenfluramine treatment at the time of the last visit had been seizure-free for at least 1 year. In total, patients had been seizure-free for a mean of 6 (1-19) years. In seven patients, the fenfluramine treatment was interrupted once during the follow-up; seizures reappeared in three of the seizure-free patients. Subsequent reintroduction of fenfluramine controlled the seizures in these three patients again. Only two patients exhibited a mild thickening of one or two cardiac valves without clinical significance.
SIGNIFICANCE:
Compared with a recent long-term follow-up series in which a maximum of 16% of patients with Dravet syndrome were seizure-free, our result of 70% of patients with Dravet syndrome remaining seizure-free is noteworthy. Given the limitations of this observational study, a larger prospective study should be undertaken to confirm these promising results.
J Child Neurol. 2012 Jul;27(7):893-7. doi: 10.1177/0883073811435325. Epub 2012 Apr 24.
Mesial temporal sclerosis in a cohort of children with SCN1A gene mutation.
Van Poppel K, Patay Z, Roberts D, Clarke DF, McGregor A, Perkins FF, Wheless JW.
Le Bonheur Comprehensive Epilepsy Program, Memphis, TN, USA.
Mesial temporal sclerosis is uncommon in childhood but has been associated with febrile status epilepticus. SCN1A gene mutations are linked to multiple epilepsy syndromes with patients frequently presenting with prolonged febrile seizures. After observing mesial temporal sclerosis in a child with SCN1A gene mutation, we retrospectively reviewed magnetic resonance imaging (MRI) findings in all patients with SCN1A gene mutation identified between 2005 and 2010. We identified 20 patients with SCN1A mutations. Six patients had evidence of definite mesial temporal sclerosis with 2 patients having bilateral abnormalities. Another 4 patients were defined as having possible mesial temporal sclerosis. This patient group revealed that 50% had findings consistent with definite or possible mesial temporal sclerosis and many did not have a history of prolonged febrile seizures. We conclude that mesial temporal sclerosis is a common finding in children with SCN1A mutations. Many of these children will have Dravet syndrome but not all.
Epilepsia. 2012 Jun;53(6):e111-4. doi: 10.1111/j.1528-1167.2012.
Different degrees of loss of function between GEFS+ and SMEI Nav 1.1 missense mutants at the same residue induced by rescuable folding defects.
Sugiura Y, Ogiwara I, Hoshi A, Yamakawa K, Ugawa Y.
Department of Neurology, Fukushima Medical University, Fukushima, Japan. y-sugiura@umin.ac.jp
Generalized epilepsy with febrile seizures plus (GEFS+) and severe myoclonic epilepsy of infancy (SMEI) differ in their clinical severity and prognosis even though mutations of the Na(v) 1.1 sodium channel are responsible for both disorders. We compared the electrophysiologic properties of two mutant Na(v) 1.1 channels characterized by distinct amino acid substitutions at the same residue position: GEFS+ (A1685V) and SMEI (A1685D). Both the mutants showed complete loss of function when expressed alone. However, the function of A1685V can be partly rescued by the β(1) subunit, consistently with a folding defect, whereas that of A1685D was not rescued. These electrophysiologic differences are consistent with the divergence in clinical severity between GEFS+ and SMEI.
Genes Brain Behav. 2012 Jun;11(4):452-60. doi: 10.1111/j.1601-183X.2012.
Confirmation of an epilepsy modifier locus on mouse chromosome 11 and candidate gene analysis by RNA-Seq.
Hawkins NA, Kearney JA.
Neuroscience Program Division of Genetic Medicine, Department of Medicine, Vanderbilt University Medical Center, Nashville, TN 37232, USA.
Epilepsy is a neurological disorder affecting approximately 1% of the worldwide population. Mutations in voltage-gated sodium channels have been identified in several monogenic epilepsy syndromes. Over 800 mutations have been identified in the voltage-gated sodium channel genes SCN1A and SCN2A in human epilepsies, including genetic epilepsy with febrile seizures plus (GEFS+) and Dravet syndrome. In GEFS+ families, affected members with the same mutation often display variability in clinical severity of the disease. This suggests that additional genes modify the effect of the primary mutation, resulting in the variable clinical presentation. The Scn2a(Q54) transgenic mouse model has an epilepsy phenotype that varies depending on the genetic strain background. Scn2a(Q54) mice congenic on the C57BL/6J strain exhibit delayed seizure onset and improved survival compared to (C57BL/6J × SJL/J)F1.Q54 mice. Two modifier loci of Scn2a(Q54) seizure susceptibility were mapped and designated Moe1 (modifier of epilepsy) on chromosome (chr) 11 and Moe2 on chr 19. To confirm Moe1 and refine its position, we generated interval-specific congenic lines carrying C57BL/6J-derived chr 11 alleles on the SJL/J strain and refined the map position to 89-104 Mb. We then used RNA-Seq for candidate analysis in the modifier region. C57BL/6J and SJL/J male and female brain RNAs were sequenced, revealing numerous significant transcriptome differences and coding single-nucleotide polymorphisms. Additional consideration of gene function and expression suggested several strong candidate modifier genes, including two voltage-gated calcium channel subunits, Cacna1g and Cacnb1, and the proline and acidic amino acid-rich basic leucine zipper transcription factor, Hlf.
Neuropediatrics. 2012 Feb;43(1):17-21. doi: 10.1055/s-0032-1307454. Epub 2012 Mar 19.
Bromide in patients with SCN1A-mutations manifesting as Dravet syndrome.
Lotte J, Haberlandt E, Neubauer B, Staudt M, Kluger GJ.
Neuropediatric Clinic and Clinic for Neurorehabilitation, Epilepsy Center for Children and Adolescents, Schön Klinik Vogtareuth, Germany. jan.lotte@web.de
We report a retrospective analysis of bromide therapy in 32 patients suffering from Dravet syndrome with SCN1A-mutations who received bromide. After 3 months of bromide treatment, 26 patients (81%) showed a relevant improvement with a reduction of seizure frequency by >50% (>75%) in 18 (12) patients (56 and 37%, respectively). After 12 months, we observed a reduction of >50% (>75%) in 15 (9) patients (47 and 28%, respectively). Long-term response was noted in 18 patients (56%). Adverse reactions were mainly mild or moderate leading to treatment termination in 5/32 patients; no aggravation was reported. We conclude that bromide holds promise in patients with SCN1A-mutations suffering from Dravet syndrome.
Epilepsy Res. 2012 Jul;100(3):252-7. doi: 10.1016/j.eplepsyres.2012.01.
Is the ketogenic diet effective in specific epilepsy syndromes?
Nangia S, Caraballo RH, Kang HC, Nordli DR, Scheffer IE.
Children’s Memorial Hospital Epilepsy Center, 2300 Children’s Plaza, Box 29, Chicago, IL 60614-3363, USA.
Is the ketogenic diet (KD) more effective in certain epilepsy syndromes? The KD has been shown to be effective in treating multiple seizure types and epilepsy syndromes. We review the effectiveness of the KD in Dravet syndrome, epilepsy with myoclonic-atonic seizures, mitochondrial disease, tuberous sclerosis, late infantile and juvenile neuronal ceroid lipofuscinosis, and febrile infection-related epilepsy syndrome. In certain epilepsy syndromes, like epilepsy with myoclonic-atonic seizures, the diet should be considered early in the course of treatment.
Arch Neurol. 2012 Jul;69(7):873-8.
Progressive gait deterioration in adolescents with Dravet syndrome.
Rodda JM, Scheffer IE, McMahon JM, Berkovic SF, Graham HK.
Department of Physiotherapy, Melbourne School of Health Sciences, University of Melbourne, Victoria, Australia.
OBJECTIVE:
To characterize changes in gait by age in patients with Dravet syndrome.
DESIGN:
Prospective, cross-sectional study.
SETTING:
Tertiary children’s hospital.
PATIENTS:
Twenty-six subjects with Dravet syndrome, aged 2 to 34 years. Twenty-three patients had mutations of the sodium channel α1 subunit gene, SCN1A.
INTERVENTIONS:
Assessment via video gait analysis, physical examination of the lower limbs, use of the Functional Mobility Scale, and radiographs of the pelvis and feet.
MAIN OUTCOME MEASURES:
Classification of the sagittal gait pattern and foot posture, assessment of muscle extensibility and joint range, and rating of functional mobility.
RESULTS:
Children aged 0 to 5 years had a normal or near-normal gait, whereas 5 of 10 children aged 6 to 12 years and 8 of 9 children aged 13 years or older had crouch gait. Physical examination showed that with increasing age, passive knee extension (P = .008) and hip extension (P = .003) decreased, external tibial torsion (P = .007) and pes planovalgus (P = .05) increased, and increased hip internal rotation did not show age-related change (P = .27). The Functional Mobility Scale showed universal independent walking over 5 and 50 m; however, adolescents showed wide variation in their ratings over 500 m, indicating mobility ranging from wheelchair use to independent walking (P = .02).
CONCLUSIONS:
Children with Dravet syndrome show progressive gait deterioration in the second decade of life, with crouch gait and skeletal malalignment comprising increased femoral neck anteversion, external tibial torsion, and pes valgus. These age-related changes have a significant impact on mobility and independence in the community setting.
Epilepsy Res. 2012 Jun;100(1-2):194-8. doi: 10.1016/j.eplepsyres.2012.02.
Febrile infection-related epilepsy syndrome is not caused by SCN1A mutations.
Carranza Rojo D, Harvey AS, Iona X, Dibbens LM, Damiano JA, Arsov T, Gill D, Freeman JL, Leventer RJ, Vincent A, Berkovic SF, McMahon JM, Scheffer IE.
Epilepsy Research Centre, Austin Health, The University of Melbourne, Heidelberg, Victoria, Australia.
Two distinctive epileptic encephalopathies, febrile infection-related epilepsy syndrome (FIRES) and Dravet syndrome (DS), present with febrile status epilepticus in a normal child followed by refractory focal seizures and cognitive decline although there are differentiating features. Abnormalities of the sodium channel gene SCN1A are found in 75% of DS patients. We found no SCN1A mutations or copy number variants in 10 patients with FIRES. Other genetic etiologies deserve consideration.
Eur J Med Genet. 2012 May;55(5):338-41. doi: 10.1016/j.ejmg.2012.01.008. Epub 2012 Jan 25.
Another cause of vaccine encephalopathy: a case of Angelman syndrome.
Novy J, Catarino CB, Chinthapalli K, Smith SM, Clayton-Smith J, Hennekam RC, Hammond P, Sisodiya SM.
Department of Clinical and Experimental Epilepsy, UCL Institute of Neurology, University College London, Queen Square, London, UK.
Dravet syndrome has been found recently as an important underlying condition in cases of alleged vaccine encephalopathy after pertussis vaccination, where vaccination seemed to have precipitated the occurrence of the disease without modifying the long-term course. We report on a patient diagnosed with Angelman syndrome in her fifth decade, in whom the intellectual disability and epilepsy had been assumed to be caused by a vaccine encephalopathy following smallpox vaccination. Clinical features of Angelman syndrome had faded away. The history of the present patient suggests that genetic conditions other than Dravet syndrome can be associated with an alleged vaccine encephalopathy. A history of vaccine encephalopathy is rare among patients with learning disability and refractory epilepsy (1.4% in our cohort), but it should lead to consideration of a comprehensive genetic work-up if Dravet syndrome is excluded. The early history of the patient, when available, should guide the investigations. Medico-legal aspects are also discussed.
Epilepsy Behav. 2012 Mar;23(3):177-86. doi: 10.1016/j.yebeh.2011.11.022. Epub 2012 Feb 16.
SCN1A mutations in Dravet syndrome: impact of interneuron dysfunction on neural networks and cognitive outcome.
Bender AC, Morse RP, Scott RC, Holmes GL, Lenck-Santini PP.
Department of Neurology, Neuroscience Center at Dartmouth, Dartmouth Medical School, Hanover, NH 03756, USA. Alex.C.Bender@Dartmouth.edu
Dravet syndrome (DS) is a childhood disorder associated with loss-of-function mutations in SCN1A and is characterized by frequent seizures and severe cognitive impairment. Animal studies have revealed new insights into the mechanisms by which mutations in this gene, encoding the type I voltage-gated sodium channel (Na(v)1.1), may lead to seizure activity and cognitive dysfunction. In this review, we further consider the function of fast-spiking GABAergic neurons, one cell type particularly affected by these mutations, in the context of the temporal coordination of neural activity subserving cognitive functions. We hypothesize that disruptions in GABAergic firing may directly contribute to the poor cognitive outcomes in children with DS, and discuss the therapeutic implications of this possibility.
Curr Opin Neurol. 2012 Apr;25(2):173-8. doi: 10.1097/WCO.0b013e3283515e4a.
Ketogenic diets: new advances for metabolism-based therapies.
Kossoff EH, Hartman AL.
Departments of Neurology and Pediatrics, The John M. Freeman Pediatric Epilepsy Center, Johns Hopkins Medical Institutions, Baltimore, Maryland, USA. ekossoff@jhmi.edu
PURPOSE OF REVIEW:
Despite myriad anticonvulsants available and in various stages of development, there are thousands of children and adults with epilepsy worldwide still refractory to treatment and not candidates for epilepsy surgery. Many of these patients will now turn to dietary therapies such as the ketogenic diet, medium-chain triglyceride diet, modified Atkins diet, and low glycemic index treatment.
RECENT FINDINGS:
In the past several years, neurologists are finding new indications to use these dietary treatments, perhaps even as first-line therapy, including infantile spasms, myoclonic-astatic epilepsy (Doose syndrome), Dravet syndrome, and status epilepticus (including FIRES syndrome). Adults are also one of the most rapidly growing populations being treated nowadays; this group of patients previously was not typically offered these treatments. In 2009, two controlled trials of the ketogenic diet were published, as well as an International Expert Consensus Statement on dietary treatment of epilepsy. Ketogenic diets are also now being increasingly studied for neurological conditions other than epilepsy, including Alzheimer’s disease and cancer. Insights from basic science research have helped elucidate the mechanisms by which metabolism-based therapy may be helpful, in terms of both an anticonvulsant and possibly a neuroprotective effect.
SUMMARY:
Dietary therapy for epilepsy continues to grow in popularity worldwide, with expanding use for adults and conditions other than epilepsy.
Epilepsia. 2012 Mar;53(3):e55-9. doi: 10.1111/j.1528-1167.2011.
Efficacy of the ketogenic diet: which epilepsies respond?
Thammongkol S, Vears DF, Bicknell-Royle J, Nation J, Draffin K, Stewart KG, Scheffer IE, Mackay MT.
Children’s Neuroscience Centre, Royal Children’s Hospital, Parkville, Victoria, Australia.
We report the efficacy of the ketogenic diet in refractory epilepsies focusing on outcomes with regard to epilepsy syndromes and etiology in children and adults with refractory epilepsy. Sixty-four consecutive children and four adults were prospectively enrolled from 2002 to 2009; seven were excluded from analysis. The classical ketogenic diet was initiated on an inpatient basis with dietary ratios ranging from 2:1 to 4:1 fat to carbohydrate and protein. Patients were classified according to syndrome and etiology using the 1989 and more recent 2010 International League Against Epilepsy (ILAE) classification systems. Responders were defined as >50% reduction in seizure frequency compared to baseline. Syndromes included symptomatic generalized (52), genetic (idiopathic) generalized (7), and focal epilepsies (2) and etiologies included structural (24), genetic (18), and unknown (19). Twenty-nine (48%) of 61 patients were responders at 3 months. Two children became seizure-free: one with focal epilepsy of unknown etiology and another with refractory childhood absence epilepsy. Responsive syndromes included migrating partial epilepsy of infancy, childhood absence epilepsy, focal epilepsy, epilepsy with myoclonic-atonic seizures, and Dravet syndrome. Children with lissencephaly and hypoxic ischemic encephalopathy had surprisingly good responses. The ketogenic diet is an effective treatment for children and adults with refractory epilepsy. The response is predicted by type of epilepsy syndrome. Accurate characterization of the electroclinical syndrome is an important factor in decisions about timing of initiation of the ketogenic diet.
Epilepsia. 2012 Mar;53(3):558-64. doi: 10.1111/j.1528-1167.2011.
Mutations of the SCN1A gene in acute encephalopathy.
Saitoh M, Shinohara M, Hoshino H, Kubota M, Amemiya K, Takanashi JL, Hwang SK, Hirose S, Mizuguchi M.
Department of Developmental Medical Sciences, Graduate School of Medicine, University of Tokyo, Tokyo, Japan. makisaito-tky@umin.net.jp
PURPOSE:
Acute encephalopathy is the most serious complication of pediatric viral infections, such as influenza and exanthema subitum. It occurs worldwide, but is most prevalent in East Asia. Recently, there have been sporadic case reports of epilepsy/febrile seizure and acute encephalopathy with a neuronal sodium channel alpha 1 subunit (SCN1A) mutation. To determine whether SCN1A mutations are a predisposing factor of acute encephalopathy, we sought to identify SCN1A mutations in a large case series of acute encephalopathy including various syndromes.
METHODS:
We analyzed the SCN1A gene in 87 patients with acute encephalopathy, consisting of 20 with acute necrotizing encephalopathy (ANE), 61 with acute encephalopathy with biphasic seizures and late reduced diffusion (AESD), and six with nonspecific (unclassified) acute encephalopathy.
KEY FINDINGS:
Three patients had distinct point mutations. Two of them had epileptic seizures prior to acute encephalopathy. Clinical and neuroradiologic findings of acute encephalopathy were diverse among the three patients, although all had a prolonged and generalized seizure at its onset. The first patient with V982L had partial epilepsy and AESD. The second patient with M1977L had febrile seizures and nonspecific acute encephalopathy. The third patient with R1575C had no seizures until the onset of ANE. M1977L was a novel mutation, whereas the remaining two, V982L and R1575C, have previously been reported in cases of Dravet syndrome and acute encephalopathy, respectively.
SIGNIFICANCE:
These findings provide further evidence that SCN1A mutations are a predisposing factor for the onset of various types of acute encephalopathy.
Tidsskr Nor Laegeforen. 2012 Jan 10;132(1):44-7. doi: 10.4045/tidsskr.11.0539.
[Dravet syndrome as a cause of epilepsy and learning disability].
[Article in Norwegian]
Lund C, Bremer A, Lossius MI, Selmer KK, Brodtkorb E, Nakken KO.
Nasjonalt kompetansesenter for sjeldne epilepsirelaterte diagnoser, Oslo universitetssykehus, Norway. caroline.lund@oslo-
BACKGROUND:
Dravet syndrome is a severe, genetic epileptic encephalopathy with seizures starting during the first year of life. We present a review of the genetic and clinical picture along with treatment aspects.
MATERIAL AND METHODS:
This review is based on a non-systematic literature search in PubMed until April 2011 and the personal experiences of the authors.
RESULTS:
Dravet syndrome should be suspected in children with febrile hemiconvulsions or tonic-clonic seizures in the first year of life. Non-febrile seizures also occur, and other seizure types gradually appear, e.g. myoclonic jerks, atypical absences or focal seizures. In adulthood the clinical picture is less characteristic. The clinical diagnosis is supported by genetic testing; 70-80% of the patients have mutations in the sodium channel subunit gene SCN1A. Seizure control is difficult to achieve, but valproate, benzodiazepines and stiripentol may cause improvement, whereas sodium channel blockers, such as lamotrigine and carbamazepine may aggravate the tendency towards seizures.
INTERPRETATION:
Dravet syndrome appears to be an under-recognised condition among both children and adults with severe epilepsy and learning disability. Clinical information from the first years of life is essential in making the diagnosis. A correct diagnosis at an early age is essential for appropriate treatment and genetic counselling.
J Pediatr. 2012 Mar;160(3):532-3. doi: 10.1016/j.jpeds.2011.11.058. Epub 2012 Jan 9.
Additional information regarding « Dravet syndrome: inroads into understanding epileptic encephalopathies ».
Kobayashi K, Ohtsuka Y, Ohmori I.
Brain Dev. 2012 Sep;34(8):617-9. doi: 10.1016/j.braindev.2011.11.
On the likelihood of SCN1A microdeletions or duplications in Dravet syndrome with missense mutation.
Shi X, Wang J, Kurahashi H, Ishii A, Higurashi N, Kaneko S, Hirose S.
Department of Pediatrics, School of Medicine, Fukuoka University, Fukuoka, Japan.
This study examines whether microdeletions and duplications of the gene encoding α1 subunit of the sodium channel (SCN1A) are underlying causes in Dravet syndrome (DS) with SCN1A missense mutation. Multiple exonic deletions were identified in 8/84 patients without mutation and 0/41 patients with missense mutations. Our findings indicate that while microdeletions are not rare in SCN1A-negative patients, they are not likely to be present simultaneously with other SCN1A mutations.
Pediatr Neurol. 2012 Jan;46(1):24-31. doi: 10.1016/j.pediatrneurol.2011.
Genes of early-onset epileptic encephalopathies: from genotype to phenotype.
Mastrangelo M, Leuzzi V.
Division of Child Neurology, Department of Pediatrics, Child Neurology, and Psychiatry, Sapienza University of Rome, Rome, Italy.
Early-onset epileptic encephalopathies are severe disorders in which cognitive, sensory, and motor development is impaired by recurrent clinical seizures or prominent interictal epileptiform discharges during the neonatal or early infantile periods. They include Ohtahara syndrome, early myoclonic epileptic encephalopathy, West syndrome, Dravet syndrome, and other diseases, e.g., X-linked myoclonic seizures, spasticity and intellectual disability syndrome, idiopathic infantile epileptic-dyskinetic encephalopathy, epilepsy and mental retardation limited to females, and severe infantile multifocal epilepsy. We summarize recent updates on the genes and related clinical syndromes involved in the pathogenesis of early-onset epileptic encephalopathies: Aristaless-related homeobox (ARX), cyclin-dependent kinase-like 5 (CDKL5), syntaxin-binding protein 1 (STXBP1), solute carrier family 25 member 22 (SLC25A22), nonerythrocytic α-spectrin-1 (SPTAN1), phospholipase Cβ1 (PLCβ1), membrane-associated guanylate kinase inverted-2 (MAGI2), polynucleotide kinase 3′-phosphatase (PNKP), sodium channel neuronal type 1α subunit (SCN1A), protocadherin 19 (PCDH19), and pyridoxamine 5-prime-phosphate oxidase (PNPO).
Genes Brain Behav. 2012 Mar;11(2):170-6. doi: 10.1111/j.1601-183X.2011.
Mosaic SCN1A mutations in familial partial epilepsy with antecedent febrile seizures.
Shi YW, Yu MJ, Long YS, Qin B, He N, Meng H, Liu XR, Deng WY, Gao MM, Yi YH, Li BM, Liao WP.
Institute of Neuroscience, The Second Affiliated Hospital of Guangzhou Medical University, Key Laboratory of Neurogenetics and Channelopathies of Guangdong Province and the Ministry of Education of China, Guangdong, China.
SCN1A is the most relevant epilepsy gene. Mutations of SCN1A generate phenotypes ranging from the extremely severe form of Dravet syndrome (DS) to a mild form of generalized epilepsy with febrile seizures plus (GEFS+). Mosaic SCN1A mutations have been identified in rare familial DS. It is suspected that mosaic mutations of SCN1A may cause other types of familial epilepsies with febrile seizures (FS), which are more common clinically. Thus, we screened SCN1A mutations in 13 families with partial epilepsy with antecedent febrile seizures (PEFS+) using denaturing high-performance liquid chromatography and sequencing. The level of mosaicism was further quantified by pyrosequencing. Two missense SCN1A mutations with mosaic origin were identified in two unrelated families, accounting for 15.4% (2/13) of the PEFS+ families tested. One of the mosaic carriers with ~25.0% mutation of c.5768A>G/p.Q1923R had experienced simple FS; another with ~12.5% mutation of c.4847T>C/p.I1616T was asymptomatic. Their heterozygous children had PEFS+. Recurrent transmission occurred in both families, as noted in most of the families with germline mosaicism reported previously. The two mosaic mutations identified in this study are less destructive missense, compared with the more destructive truncating and splice-site mutations identified in the majority of previous studies. This is the first report of mosaic SCN1A mutations in families with probands that do not exhibit DS, but manifest only a milder phenotype. Therefore, such families with mild cases should be approached with caution in genetic counseling and the possibility of mosaicism origin associated with high recurrence risk should be excluded.
Epilepsia. 2012 Jan;53(1):87-100. doi: 10.1111/j.1528-1167.2011.
Pure haploinsufficiency for Dravet syndrome Na(V)1.1 (SCN1A) sodium channel truncating mutations.
Bechi G, Scalmani P, Schiavon E, Rusconi R, Franceschetti S, Mantegazza M.
Department of Neurophysiopathology, Besta Foundation Neurological Institute, Milan, Italy.
PURPOSE:
Dravet syndrome (DS), a devastating epileptic encephalopathy, is mostly caused by mutations of the SCN1A gene, coding for the voltage-gated Na(+) channel Na(V)1.1 α subunit. About 50% of SCN1A DS mutations truncate Na(V)1.1, possibly causing complete loss of its function. However, it has not been investigated yet if Na(V)1.1 truncated mutants are dominant negative, if they impair expression or function of wild-type channels, as it has been shown for truncated mutants of other proteins (e.g., Ca(V) channels). We studied the effect of two DS truncated Na(V)1.1 mutants, R222* and R1234*, on coexpressed wild-type Na(+) channels.
METHODS:
We engineered R222* or R1234* in the human cDNA of Na(V)1.1 (hNa(V)1.1) and studied their effect on coexpressed wild-type hNa(V)1.1, hNa(V)1.2 or hNa(V)1.3 cotransfecting tsA-201 cells, and on hNa(V)1.6 transfecting an human embryonic kidney (HEK) cell line stably expressing this channel. We also studied hippocampal neurons dissociated from Na(V)1.1 knockout (KO) mice, an animal model of DS expressing a truncated Na(V)1.1 channel.
KEY FINDINGS:
We found no modifications of current amplitude coexpressing the truncated mutants with hNa(V)1.1, hNa(V)1.2, or hNa(V)1.3, but a 30% reduction coexpressing them with hNa(V)1.6. However, we showed that also coexpression of functional full-length hNa(V)1.1 caused a similar reduction. Therefore, this effect should not be involved in the pathomechanism of DS. Some gating properties of hNa(V)1.1, hNa(V)1.3, and hNa(V)1.6 were modified, but recordings of hippocampal neurons dissociated from Na(V)1.1 KO mice did not show any significant modifications of these properties. Therefore, Na(V)1.1 truncated mutants are not dominant negative, consistent with haploinsufficiency as the cause of DS.
SIGNIFICANCE:
We have better clarified the pathomechanism of DS, pointed out an important difference between pathogenic truncated Ca(V)2.1 mutants and hNa(V)1.1 ones, and shown that hNa(V)1.6 expression can be reduced in physiologic conditions by coexpression of hNa(V)1.1. Moreover, our data may provide useful information for the development of therapeutic approaches.
J Child Neurol. 2012 Jul;27(7):914-6. doi: 10.1177/0883073811426933. Epub 2011 Dec 2.
Thoracic myelopathy secondary to seizure following scoliosis surgery.
Myers KA, Payne ET, Esser MJ, Kirton A, Howard JJ.
Department of Pediatrics, Division of Neurology, Alberta Children’s Hospital, Calgary, Alberta, Canada. kmyers@ucalgary.ca
The incidence of spinal injuries is increased in people with epilepsy although compressive thoracic myelopathy has not been reported. We describe a 15-year-old girl with SCN1A mutation (Dravet syndrome), refractory generalized tonic-clonic seizures, and prior posterior instrumentation and fusion for scoliosis, who presented with progressive lower extremity weakness. Junctional kyphosis with disc herniation and spinal cord compression directly rostral to the instrumentation was apparent on imaging. On history, the patient had suffered a particularly severe convulsive seizure just before developing symptoms. Surgical decompression and stabilization led to a complete neurologic recovery. This unusual presentation of myelopathy illustrates the need to consider this complication in patients with epilepsy and spinal instrumentation.
An Pediatr (Barc). 2012 Apr;76(4):218-23. doi: 10.1016/j.anpedi.2011.10.001. Epub 2011 Nov 21.
[Febrile seizures in the first year of life: Dravet spectrum epilepsy?].
[Article in Spanish]
Sánchez-Carpintero R, Núñez MT, Aznárez N, Narbona García J.
Unidad de Neurología Infantil, Departamento de Pediatría, Clínica Universidad de Navarra, Pamplona, España. rsanchezc@unav.es
INTRODUCTION:
Dravet syndrome is a drug resistant epilepsy which starts in the first year of life with febrile seizures, followed by cognitive impairment and epilepsy with multiple seizure types. Diagnosis has been typically made at the age of three to four years, but earlier diagnosis is now possible as clinical features are better recognised and molecular diagnosis is available.
PATIENTS AND METHODS:
We studied a series of 14 children with Dravet syndrome or Dravet spectrum epilepsy. A screening test, developed by other authors to distinguish the febrile seizures in Dravet syndrome from febrile seizures from other origin, was applied to the clinical features of the seizures occurring during the first year of life in our patients.
RESULTS:
Clinical suspicion of Dravet spectrum epilepsy was possible in 100% of children in our series. Moreover, taking into consideration only the first seizure, 79% of patients scored sufficiently to detect Dravet syndrome.
CONCLUSIONS:
Dravet syndrome can be recognised during the first year of life. It is important that physicians are made aware of these clinical criteria capable to distinguish febrile seizures in Dravet syndrome from febrile seizures of other origin, and set up a protocol to collect appropriate data regarding febrile seizures occurring in the first year of life.
Med Hypotheses. 2012 Feb;78(2):247-9. doi: 10.1016/j.mehy.2011.10.037. Epub 2011 Nov 17.
Are SCN1A gene mutations responsible for genetic susceptibility to subacute sclerosing panencephalitis?
Garg RK.
Department of Neurology, Chhatrapati Shahuji Maharaj Medical University, Uttar Pradesh, Lucknow, India. garg50@yahoo.com
Dravet syndrome, characterized predominantly by myoclonus, has a striking clinical resemblance to subacute sclerosing panencephalitis (SSPE). Patients with Dravet syndrome develop significant mental decline with advancing age of affected child like in SSPE. It is well established that SCN1A gene mutations are associated with Dravet syndrome. Even periodic EEG complexes have been described in Dravet syndrome. In addition to Dravet syndrome, several other types of acute and subacute encephalopathic syndromes having clinical and electroencephalographic resemblance to SSPE are associated with SCN1A gene mutations. SSPE is a devastating progressive inflammatory disorder of the central nervous system. It is caused by persistent infection of the brain by an aberrant measles virus. Only a few of a vast number of measles infected pediatric population develop SSPE. There are several reports describing presence of SSPE is close relatives and it has been described previously in sibling and twin pairs. A genetic susceptibility for development of SSPE is likely. In fact, a variety of genetic abnormalities have already been described in patients with SSPE. It can also be argued that because of striking clinical resemblance between Dravet and various epileptic and encephalopathic syndromes associated with SCN1A gene mutations and SSPE, SCN1A gene abnormalities may also be responsible for susceptibility to SSPE in measles infected children.
Epilepsia. 2012 Jan;53(1):79-86. doi: 10.1111/j.1528-1167.2011.
Acute encephalopathy in children with Dravet syndrome.
Okumura A, Uematsu M, Imataka G, Tanaka M, Okanishi T, Kubota T, Sudo A, Tohyama J, Tsuji M, Ohmori I, Naiki M, Hiraiwa-Sofue A, Sato H, Saitoh S, Shimizu T.
Department of Pediatrics, Juntendo University Faculty of Medicine, Bunkyo-ku, Tokyo, Japan. okumura@juntendo.ac.jp
PURPOSE:
The occurrence of acute encephalopathy in children with Dravet syndrome has been reported sporadically. This study clarified the features of acute encephalopathy in children with Dravet syndrome.
METHODS:
Through the mailing list of the Annual Zao Conference on Pediatric Neurology, we collected 15 patients with clinically diagnosed Dravet syndrome, who had acute encephalopathy, defined as a condition with decreased consciousness with or without other neurologic symptoms, such as seizures, lasting for >24 h in association with infectious symptoms.
KEY FINDINGS:
There were seven boys and eight girls. A mutation of the SCN1A gene was present in nine (truncation in six and missense in three). The frequency of seizures during the 3 months before the onset of acute encephalopathy was monthly in seven children and none in three. The median age at the onset of acute encephalopathy was 44 months (range 8-184 months). All children had status epilepticus followed by coma as the initial manifestation. Two different distributions of brain lesions were observed on diffusion-weighted images during the acute phase: cerebral cortex-dominant lesions with or without deep gray matter involvement and subcortical-dominant lesions. Four children died; nine survived with severe sequelae, and two had moderate sequelae.
SIGNIFICANCE:
We must be aware that acute encephalopathy is an important complication in children with Dravet syndrome, and associated with fulminant clinical manifestations and a poor outcome.
Epilepsy Res. 2012 Mar;99(1-2):21-7. doi: 10.1016/j.eplepsyres.2011.10.
Early clinical features in Dravet syndrome patients with and without SCN1A mutations.
Petrelli C, Passamonti C, Cesaroni E, Mei D, Guerrini R, Zamponi N, Provinciali L.
Neurology Clinic, Polytechnic University of Marche, Ancona, Italy. cristinapetrelli84@alice.it
BACKGROUND:
SCN1A is the most clinically relevant epilepsy gene, most mutations causing Dravet syndrome (also known as severe myoclonic epilepsy of infancy or SMEI). We evaluated clinical differences, if any, between young patients with and without a SCN1A mutations and a definite clinical diagnosis of Dravet syndrome.
METHODS:
Twenty-five patients with a diagnosis of Dravet Syndrome (7 males, 18 females; mean age at inclusion: 10.3; median: 9±7; range: 18 months-30 years) were retrospectively studied. A clinical and genetic study focusing on SCN1A was performed, using DHPLC, gene sequencing and MLPA to detect genomic deletions/duplications. A formal cognitive and behavioral assessment was available for all patients.
RESULTS:
Analysis revealed SCN1A mutations comprising missense, truncating mutations and genomic deletions/duplications in eighteen patients and no mutation in seven. The phenotype of mutation positive patients was characterized by a higher number of seizures/month in the first year of life, an earlier seizure onset and a higher frequency of episodes of status epilepticus. The cognitive and behavioral profile was slightly worst in mutation positive patients.
CONCLUSIONS:
These findings confirm that SCN1A gene mutations are strongly associated to a more severe phenotype in patients with Dravet syndrome.
Epilepsy Res. 2012 Mar;99(1-2):28-37. doi: 10.1016/j.eplepsyres.2011.10.
PCDH19 mutation in Japanese females with epilepsy.
Higurashi N, Shi X, Yasumoto S, Oguni H, Sakauchi M, Itomi K, Miyamoto A, Shiraishi H, Kato T, Makita Y, Hirose S.
Department of Pediatrics, School of Medicine, Fukuoka University, 7-45-1, Nanakuma, Jonan-ku, Fukuoka 814-0180, Japan.
PURPOSE:
To determine the significance of PCDH19 mutations in Japanese females with epilepsy and to delineate their phenotypes.
METHODS:
PCDH19 sequencing analysis was performed in 116 females with various epilepsies, including 97 with Dravet syndrome (83.6%). They were referred for SCN1A analysis, and 52 carried SCN1A mutations.
RESULTS:
Seven heterozygous mutations in exon 1 were identified in 7 patients (6.0%): 2 frameshift, 2 nonsense, and 3 missense mutations. One patient was a monozygotic twin, and her sister with mild phenotype carried the same mutation. The main clinical features among these 8 patients included early seizure onset (≤25 months of age), seizure clusters (7/8), fever-associated seizures (7/8), single seizure type (6/8), and late deterioration of intellect (5/8). Seizure durations were generally up to a few minutes, and only one patient developed status epilepticus once. The main seizure types were generalized tonic-clonic (4/8), tonic (3/8) and focal seizures, with (2/8) or without secondary generalization (3/8). Myoclonic, atonic and absence seizures were extremely rare. Two patients had Dravet syndrome (25%), and this proportion was significantly smaller than that in the total subjects (p<0.01).
CONCLUSION:
PCDH19 mutation is a relatively frequent cause of epilepsy in Japanese females. Dravet syndrome was rare in our cohort.
Acta Neurol Scand. 2012 May;125(5):359-62. doi: 10.1111/j.1600-0404.2011.
Dravet syndrome–considerable delay in making the diagnosis.
Bremer A, Lossius MI, Nakken KO.
Division of Surgery and Neuroscience, National Centre for Epilepsy, Oslo University Hospital, Norway.anna.bremer@vestreviken.no
OBJECTIVES:
To assess delay in diagnosis and clinical characteristics of Dravet syndrome based on the Dravet register at The National Centre for Epilepsy in Norway.
MATERIAL AND METHODS:
Medical records of patients diagnosed with Dravet syndrome since 2007 were analysed.
RESULTS:
Twenty-two patients were identified. In 15, genetic screening disclosed mutations/deletions in the SCN1A gene. Average time from seizure onset to diagnosis was 7.4 years. Mean age at seizure onset was 6.7 months, nine had hemiconvulsions and 13 had generalized tonic-clonic seizures. The seizures were precipitated by fever in 17, by external heating in three. During second year of life, multiple seizure types and cognitive and motoric stagnation occurred. No patients became seizure-free with antiepileptic drugs. The effect of vagal nerve stimulation was disappointing.
CONCLUSIONS:
By making an early diagnosis, an extensive presurgical evaluation may be avoided, and the patient and their parents may be offered genetic guidance.
Brain Dev. 2012 Aug;34(7):541-5. doi: 10.1016/j.braindev.2011.09.
Clinical spectrum of SCN2A mutations.
Shi X, Yasumoto S, Kurahashi H, Nakagawa E, Fukasawa T, Uchiya S, Hirose S.
Department of Pediatrics, School of Medicine, Fukuoka University, Nanakuma, Fukuoka, Japan.
Mutations in SCN2A, the gene encoding α2 subunit of the neuronal sodium channel, are associated with a variety of epilepsies: benign familial neonatal-infantile seizures (BFNIS); genetic epilepsy with febrile seizures plus (GEFS+); Dravet syndrome (DS); and some intractable childhood epilepsies. More than 10 new mutations have been identified in BFNIS, all of them are missense. To date, only one nonsense mutation has been found in a patient with intractable childhood epilepsy and severe mental decline. Recently, microduplication of chromosome 2q24.3 (containing eight genes including SCN2A, SCN3A, and the 3′ end of SCN1A) was reported in a family with dominantly inherited neonatal seizures and intellectual disability. Functional studies of SCN2A mutations show that they can cause divergent biophysical defects in Na(V)1.2 and impair cell surface expressions. There is no consistent relationship between genotype and phenotype.
J Child Neurol. 2012 Apr;27(4):439-44. doi: 10.1177/0883073811419262. Epub 2011 Oct 21.
Electroencephalographic features in dravet syndrome: five-year follow-up study in 22 patients.
Specchio N, Balestri M, Trivisano M, Japaridze N, Striano P, Carotenuto A, Cappelletti S, Specchio LM, Fusco L, Vigevano F.
Division of Neurology, Bambino Gesù Children’s Hospital, IRCCS, Rome, Italy. nicola.specchio@opbg.net
The aim of the study was to evaluate interictal electroencephalogram features in 22 patients with Dravet syndrome from the onset of the disease through the next 5 years. Electroencephalogram was abnormal in 5 patients (22.7%) at onset, and in 17 (77.3%) at the end of the study. Epileptiform abnormalities (focal, multifocal, or generalized) were seen in 6 patients at the onset and in 14 (27% vs 64%) at the end of the study. Photoparoxysmal response was present in 41% of patients at the end of follow-up. No statistical differences were found between mutated and nonmutated groups regarding evolution of background activity, interictal abnormalities, and presence of photoparoxysmal response. Electroencephalogram findings seemed to be age dependent, variable among different patients, and not influenced by the presence of sodium channel, voltage-gated, type I, alpha subunit (SCN1A) mutation. The lack of specific epileptiform abnormalities contributes to the difficulty of patients’ management in Dravet syndrome.
Brain Dev. 2012 Jun;34(6):469-77. doi: 10.1016/j.braindev.2011.08.
Maturation of EEG oscillations in children with sodium channel mutations.
Holmes GL, Bender AC, Wu EX, Scott RC, Lenck-Santini PP, Morse RP.
Department of Neurology, Neuroscience Center at Dartmouth, Dartmouth Medical School, Hanover, NH 03756, USA. Gregory.L.Holmes@Dartmouth.Edu
Dravet syndrome (DS) is a severe epileptic encephalopathy beginning in infancy in which children have difficult to control seizures and cognitive impairment. The majority of children with DS carry mutations of the gene Scn1a, which codes for the alpha subunit of the type 1 voltage-gated sodium channel and is important for the function of interneurons. Interneurons have a critical role in the generation of brain rhythms involved in cognitive processing. We hypothesized that children with DS with Scn1a mutations would have abnormal oscillatory activity. To address this hypothesis, we used EEG power spectral analysis during the wakening to determine if frequency and power are altered in 23 EEGs from 12 children with DS compared to 18 age-matched controls. While there were few differences between the EEG power spectra in DS and controls in children under 2years, in older children group differences were apparent. In DS children between 3 and 5years there were significant decreases in percentage of alpha power compared to controls and in DS children over age 6years there was a marked increase of theta and decrease of alpha compared to controls. Developmental status paralleled the power spectral analysis with an increasing likelihood of having severe cognitive problems with increasing age. These results demonstrate that Scn1a mutations result in an age-dependent alteration in oscillatory process. Such abnormalities in developmental progression of oscillations may play an important role in poor cognitive development in children with DS.
Seizure. 2012 Jan;21(1):17-20. doi: 10.1016/j.seizure.2011.08.010. Epub 2011 Sep 8.
Dravet syndrome: patients with co-morbid SCN1A gene mutations and mitochondrial electron transport chain defects.
Craig AK, de Menezes MS, Saneto RP.
Division of Pediatric Neurology, Seattle Children’s Hospital/University of Washington, 4800 Sand Point Way NE, Seattle, WA 98105, United States.
PURPOSE:
To review our cohort of patients with Dravet syndrome and determine if patients with SCN1A mutations can also express mitochondrial disease due to electron transport chain dysfunction.
METHODS:
A retrospective chart review was used to describe clinical manifestations and retrieve biochemical testing, neuroimaging, gene sequencing, and electroencephalographic results of patients expressing both mitochondrial disease and Dravet syndrome.
RESULTS:
Two children were found to have pathological mutations in the SCN1A gene and defects in mitochondrial electron transport chain complex activity. Both developed early febrile and medically intractable afebrile seizures with resulting neurocognitive decline. In the first patient, a muscle biopsy demonstrated complex IV dysfunction and in the second patient, complex III dysfunction. Patient 1 had more difficult to control seizures, and had features consistent with severe autism. Patient 2, who had earlier control and less severe seizures, did not have features of autism. Patient 1 had SCN1A missense mutation, c. 3734 G>A and patient 2 had a mutation, c. 3733 C>T, which produces a truncation mutation.
CONCLUSION:
Our two patients underscore the need to rule out possible co-morbid mitochondrial disease and Dravet syndrome. The treatment of seizures for each is different, with valproic acid being first line treatment in Dravet syndrome and contraindicated in many mitochondrial diseases, due to possible induction of liver failure and death. Failure to pursue complete diagnostic evaluation might influence medication choice, possible seizure control, and developmental outcomes.