![]()
Ce mois-ci, 33 articles sont parus, dont :
- 6 articles dans Developmental Medecine & Child Neurology (Update on Dravet Syndrome: 9th European Congress on Epileptology, Rhodes, June 2010).
- 21 articles dans Epilepsia (Special Issue: Severe Myoclonic Epilepsy – Dravet Syndrome: Thirty Years Later, Proceedings of an international workshop. October 4-5, 2009. Verona, Italy)
Les articles ne sont pas tous traduits….Bonne lecture !
Biochem Biophys Res Commun. 2011 May 20;408(4):654-7. Epub 2011 Apr 21.
A putative disease-associated haplotype within the SCN1A gene in Dravet syndrome.
Fendri-Kriaa N, Boujilbene S, Kammoun F, Mkaouar-Rebai E, Mahmoud AB, Hsairi I, Rebai A, Triki C, Fakhfakh F.
Laboratoire de Génétique Moléculaire Humaine, Faculté de Médecine de Sfax, Université de Sfax, Tunisia.
Un haplotype putatif associé à la maladie au sein du gène SCN1A dans le syndrome de Dravet.
Le syndrome de Dravet (DS), précédemment connu sous le nom d’épilepsie myoclonique sévère du nourrisson, est l’une des formes les plus sévères d’épilepsie infantile. Le DS est causé par une mutation dans la sous-unité alpha du canal sodium voltage-dépendant du gène (SCN1A). Cependant, 25-30% des patients atteints de DS sont négatifs pour le dépistage de la mutation SCN1A, suggérant que d’autres mécanismes moléculaires peuvent expliquer ces troubles. Récemment, le premier cas de DS causé par une mutation dans la sous-unité beta du canal sodium voltage-dépendant du gène (SCN1B) a également été rapporté. Dans ce rapport, notre but est de réaliser l’analyse moléculaire des gènes SCN1A et SCN1B chez deux patients tunisiens atteints de DS. Les gènes SCN1A et SCN1B ont été analysés par séquençage direct. Aucune mutation n’a été révélée dans les gènes SCN1A et SCN1B par les analyses de séquençage. D’autre part, 11 polymorphismes mononucléotides connus ont été identifiés dans le gène SCN1A et sont composés d’un haplotype putatif associé à la maladie chez les patients avec un phénotype DS. Un des deux patients atteints de la maladie associée à un haplotype putatif du SCN1A avait aussi un polymorphisme mononucléotide connu dans le gène SCN1B. Les analyses de séquençage du gène SCN1A ont révélé la présence d’un haplotype putatif associé à la maladie chez deux patients atteints du syndrome de Dravet.
Epilepsia. 2011 Apr;52 Suppl 2:1-104.
Dravet syndrome. Proceedings of an international workshop. October 4-5, 2009. Verona, Italy.
[No authors listed]
J Child Neurol. 2011 Jun;26(6):782-5. Epub 2011 Apr 27.
Leber’s hereditary optic neuropathy mutations associated with infantile-onset myoclonic epilepsy.
Frye RE.
Division of Child and Adolescent Neurology, Department of Pediatrics, and Children’s Learning Institute, University of Texas Health Science Center, Houston, TX 77030, USA. Richard.e.frye@uth.tmc.edu
Les syndromes épileptiques qui apparaissent dans la première année de vie, surtout lorsqu’ils incluent des caractéristiques myocloniques, ont une signification particulière car ils sont associés à long terme à des anomalies développementales et neurologiques. L’épilepsie myoclonique sévère du nourrisson (syndrome de Dravet) est particulièrement intéressante car elle est associée à des crises provoquées par la fièvre et à des mutations de la sous-unité alpha du canal sodique (SCN1A) dans environ un tiers des cas. Nous rapportons ici deux enfants qui avaient des caractéristiques cliniques de l’épilepsie myoclonique sévère du nourrisson, sans mutations du gène SCN1A et à qui l’on a décelé des mutations d’ADN mitochondrial associées à la neuropathie optique héréditaire de Leber. Ces deux enfants ont montré des marqueurs de la dysfonction mitochondriale, résistant aux médicaments épileptiques, et un dysfonctionnement des systèmes non neurologique. Ces cas montrent que des mutations d’ADN mitochondrial, en particulier celles associées à la neuropathie optique héréditaire de Leber, doivent être envisagées dans les cas d’épilepsie myoclonique débutant dans l’enfance, surtout lorsque des mutations dans le gène SCN1A ne sont pas trouvées.
Dev Med Child Neurol. 2011 Apr;53 Suppl 2:19-23. doi: 10.1111/j.1469-8749.2011.03968.x.
Overall management of patients with Dravet syndrome.
Ceulemans B.
Department of Neurology-Child Neurology, University Hospital and University of Antwerp, Belgium. berten.ceulemans@uza.be
Dravet syndrome, or as it was called in the past ‘severe myoclonic epilepsy in infancy’, is a drug-resistant epilepsy first described by Charlotte Dravet in 1978. Besides the well-known and well-described therapy resistance, Dravet syndrome dramatically impacts the development and behaviour of the affected children. As it is still not a curable disease, families need to be taught how to cope with the disorder and will require assistance from both clinical and non-clinical structures. At the onset of the disease, many questions arise regarding the diagnosis of Dravet syndrome, the severity of the illness and its deleterious effects, and the management of seizures, especially the long-lasting status epilepticus. Once the diagnosis has been established, severe convulsions, often unpredictable and long-lasting, are still a major worry, but developmental and behavioural problems also rapidly become a serious concern. Later on, nearly all parents will have a child who becomes an adult with special needs, requiring specialised attention from professionals.
Dev Med Child Neurol. 2011 Apr;53 Suppl 2:16-8. doi: 10.1111/j.1469-8749.2011.03967.x.
Current therapeutic procedures in Dravet syndrome.
Chiron C.
Inserm, U663, Paris, Université Paris Descartes, Paris, France. catherine.chiron2@gmail.com
Dravet syndrome is a highly pharmaco-resistant form of epilepsy. Valproate and benzodiazepines are the first-line treatment but are usually insufficient therapeutic options. Lamotrigine, carbamazepine and high doses of intravenous phenobarbital can aggravate seizures and should be avoided. Topiramate, levetiracetam, bromide and ketogenic diet also provide substantial efficacy as adjunctive therapy and procedures. Stiripentol is the only new drug to demonstrate efficacy when combined with valproate and clobazam, as shown in two independent double-blind controlled trials dedicated to Dravet children. In order to avoid side effects (mainly loss of appetite and loss of weight) resulting from the inhibition of cytochromes P450 by stiripentol, the prescribed doses of valproate and clobazam should be reduced. Stiripentol has a proper antiepileptic effect and enhances GABAergic neurotransmission by acting on the alpha-3 subunit of GABA(A) receptors. Stiripentol was approved as an orphan drug in Europe in 2007 for adjunctive therapy in Dravet syndrome. More than 500 Dravet patients have currently been satisfactorily treated and recent experiments in Japan have confirmed stiripentol’s benefit. In practice, valproate should be initiated at the first onset of complicated febrile seizure in Dravet patients. Relapses justify the addition of clobazam and stiripentol when available. Topiramate and a ketogenic diet are alternatives in pharmaco-resistant cases.
Dev Med Child Neurol. 2011 Apr;53 Suppl 2:11-5. doi: 10.1111/j.1469-8749.2011.03966.x.
Dravet syndrome and SCN1A gene mutation related-epilepsies: cognitive impairment and its determinants.
Guerrini R, Falchi M.
Paediatric Neurology Unit and Laboratories, Children’s Hospital A. Meyer-University of Florence, Viale Pieraccini, Firenze, Italy. r.guerrini@meyer.it
Some studies have demonstrated that cognitive decline occurs in Dravet syndrome, starting shortly after the onset of seizures, rapidly progressing and then plateauing within a few years. It is unclear whether children that develop the syndrome had entirely normal cognitive skills before seizure onset, since subtle impairment easily escapes recognition in small infants. It is also difficult to demonstrate whether a recognisable profile of cognitive impairment or a definite behavioural phenotype exists. No clear-cut imaging or neuropathological marker or substrate has been recognised for cognitive impairment in this syndrome. However, there are different potentially causative factors, including the specific effects on the Nav1.1 channels caused by the underlying genic or genomic defect; frequent and prolonged convulsive and non-convulsive seizures or status epilepticus; recurrent subtle ictal phenomena, such as that accompanying pronounced visual sensitivity; the use of antiepileptic drugs with cognitive side effects, especially in heavy multiple-drug therapy; and the restrictions that children with severe epilepsy inevitably undergo.
Dev Med Child Neurol. 2011 Apr;53 Suppl 2:7-10. doi: 10.1111/j.1469-8749.2011.03965.x.
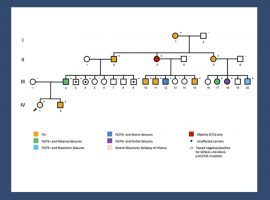
Molecular genetics of Dravet syndrome.
Neurogenetic Group, VIB Department of Molecular Genetics, University of Antwerp, Belgium. peter.dejonghe@molgen.vib-ua.be
Before the advent of molecular genetics, the nature of Dravet syndrome remained largely obscure, and arguments in favour of either an acquired origin, such as the occurrence of Dravet syndrome after vaccination, or an inherited origin, such as the occurrence of epilepsy in relatives, were formulated. In 2001 we demonstrated that the majority of Dravet patients have a genetic cause due to loss-of-function mutations in the SCN1A gene. Understandably, since this syndrome severely affects reproductive fitness, these mutations almost exclusively arise de novo, with the rare exceptions of mosaic mutations in a non-affected transmitting parent. Besides classical Sanger sequencing, mutation analysis of the SCN1A gene also requires a method that allows the detection of genomic rearrangements (MAQ, MLPA), since microdeletions or whole gene deletions also result in Dravet syndromes. Depending on the series reported and their recruitment strategies, the yield of SCN1A mutations detected varied from 50 to 80%, implying that other genes or factors must be involved in these ‘SCN1A-negative Dravet patients’. Recently mutations in some other genes have been described in these genuine Dravet patients who do not carry an SCN1A mutation. The second most important Dravet-associated gene is PCDH19.These patients initially may have all characteristics of Dravet syndrome but may later run a somewhat different course.
Dev Med Child Neurol. 2011 Apr;53 Suppl 2:1-6. doi: 10.1111/j.1469-8749.2011.03964.x.
Dravet syndrome history.
Centre Saint-Paul-Hôpital Henri Gastaut, Marseille, France. charlotte.dravet@free.fr
Severe myoclonic epilepsy of infancy (SMEI) is a complex form of epilepsy that was first described in France in 1978. Because the myoclonic component of this epilepsy is not always present and because some variability has been observed in the symptomatology, the name was changed to Dravet syndrome in 1989. The genetic aetiology of this epilepsy was discovered in 2001, and since then numerous studies have contributed to a better knowledge of the disease. Around 70% of affected patients are carriers of a mutation on the alpha subunit of the SCN1A gene. An accurate analysis of the clinical features leads to the distinction between typical and atypical forms, both with the same unfavourable prognosis and the same genetic background. However, many studies are being conducted in order to establish correlations between phenotypes and genotypes, and to understand the factors underlying the cognitive impairment of the affected patients.
Dev Med Child Neurol. 2011 Apr;53 Suppl 2:v-vi. doi: 10.1111/j.1469-8749.2011.03963.x.
Update on Dravet syndrome.
Covanis A.
Epilepsia. 2011 Apr 11. doi: 10.1111/j.1528-1167.2011.03053.x. [Epub ahead of print]
Retrospective multiinstitutional study of the prevalence of early death in Dravet syndrome.
Sakauchi M, Oguni H, Kato I, Osawa M, Hirose S, Kaneko S, Takahashi Y, Takayama R, Fujiwara T.
Department of Pediatrics, Tokyo Women’s Medical University, Tokyo, Japan Department of Pediatrics, School of Medicine, Fukuoka University, Fukuoka, Japan Department of Neuropsychiatry, School of Medicine, Hirosaki University, Aomori, Japan National Epilepsy Center, Shizuoka Institute of Epilepsy and Neurological Disorder, Shizuoka, Japan.
Purpose: A questionnaire survey was conducted in Japan to investigate the causes and prevalence of death related to Dravet syndrome. Methods: A questionnaire was delivered to 246 hospitals at which physicians were treating childhood epilepsy to gain information about the total number of patients with Dravet syndrome and their prevalence of early death. Key Findings: Responses to the survey were collected from 91 hospitals, and a total of 63 of 623 patients with Dravet syndrome died. Data from 59 of these patients were analyzed. The patients’ ages at death ranged from 13 months to 24 years and 11 months, with a median age of 6 years and 8 months. The analysis showed that the risk of mortality remained high up to approximately 12 years of age. The causes of mortality included sudden death in 31 patients (53%), acute encephalopathy with status epilepticus (SE) in 21 patients (36%), drowning in 6 patients (10%), and acute hepatopathy in one patient (1%). The incidence of sudden death reached a first peak at 1-3 years of age and reached a second peak at 18 years and older. In contrast, the incidence of acute encephalopathy with SE reached a sharp peak at 6 years of age. Seven of 10 patients who underwent an SCN1A mutation analysis exhibited positive mutations without a specific mutation site. Significance: In the present study, the prevalence of Dravet syndrome-related mortality was 10.1%. The incidence of sudden death and acute encephalopathy with SE was the highest in infancy (1-3 years) and at early school ages (with a peak at 6 years), respectively. After approximately 12 years of age, the risk of mortality declined sharply. Neither the treatment nor the number of seizures was associated with any cause of mortality. In addition, it is difficult to predict which factors lead to a fatal outcome.
Epilepsia. 2011 May;52(5):1010-7. doi: 10.1111/j.1528-1167.2011.03046.x. Epub 2011 Apr 11.
Therapy for hyperthermia-induced seizures in Scn1a mutant rats.
Hayashi K, Ueshima S, Ouchida M, Mashimo T, Nishiki T, Sendo T, Serikawa T, Matsui H, Ohmori I.
Department of Physiology, Graduate School of Medicine, Dentistry, and Pharmaceutical Sciences, Okayama University, Okayama, Japan Department of Pharmacy, Okayama University Hospital, Okayama, Japan Department of Molecular Genetics, Graduate School of Medicine, Dentistry, and Pharmaceutical Sciences, Okayama University, Okayama, Japan Institute of Laboratory Animals, Graduate School of Medicine, Kyoto University, Kyoto, Japan.
Thérapie pour les convulsions provoquées part l’hyperthermie chez des rats mutants SCN1A.
But: Les mutations dans le gène SCN1A, qui code pour la sous-unité α1 des canaux sodiques voltage-dépendants, provoquent l’épilepsie généralisée avec convulsions fébriles plus (GEFS +) et l’épilepsie myoclonique sévère du nourrisson (EMSN). Les rats mutants N1417H-SCN1A sont considérés comme un modèle animal de l’homme FS + ou GEFS +. Pour évaluer la validité de ce modèle pharmacologique, nous avons comparé les efficacités de huit médicaments antiépileptiques (MAE) différents pour le traitement des crises provoquées par l’hyperthermie en utilisant des rats mutants N1417H-SCN1A .
Méthode: Les MAE utilisés dans cette étude ont inclus le valproate, la carbamazépine (CBZ), le phénobarbital, la gabapentine, l’acétazolamide, le diazépam (DZP), le topiramate et le bromure de potassium (KBr). Les effets de ces antiépileptiques ont été évalués en utilisant le modèle de l’eau chaude, qui est un modèle de FS expérimental. Des rats agés de cinq semaines ont été pré-traités avec chaque MAE et immergé dans de l’eau à 45 ° C pour induire une hyperthermie provoquant des crises. Les crises et l’enregistrement vidéo-électroencéphalographique ont été évalués. Par ailleurs, les effets de chaque MAE sur la coordination motrice et l’équilibre ont été évalués en utilisant le test de balance-beam.
Principales conclusions: Le KBr réduit considérablement la durée des crises, et ses effets anticonvulsivants ont été comparables à ceux du DZP. D’autre part, la CBZ a diminué le seuil épileptogène. En outre, le DZP contrairement au KBr a montré une altération significative de la coordination motrice et de l’équilibre.
Signification: Le DZP et le KBr ont montré de puissants effets inhibiteurs contre les crises provoquées par l’hyperthermie chez les rats mutants SCN1A, alors que la CBZ a présenté des effets indésirables. Ces réponses aux crises provoquées par l’hyperthermie ont été similaires à ceux des patients GEFS + et EMSN. Les rats mutants N1417H-SCN1A peuvent, par conséquent, être utile pour tester l’efficacité des nouveaux antiépileptiques contre FS des patients GEFS + et EMSN.
Epilepsy Res. 2011 Jun;95(1-2):86-93. Epub 2011 Apr 6.
Neuropsychological development in children with Dravet syndrome.
Chieffo D, Battaglia D, Lettori D, Del Re M, Brogna C, Dravet C, Mercuri E,Guzzetta F.
Child Neurology and Psychiatry, Catholic University, Rome, Italy.
Développement neuropsychologique d’enfants atteints du syndrome de Dravet
OBJECTIF: Le but de cette étude est de rapporter un profil détaillé du développement neuropsychologique chez les enfants atteints du syndrome de Dravet .
MÉTHODES: Douze enfants avec un syndrome de Dravet ont été évalués à l’aide d’une évaluation cliniques et neuropsychologiques détaillée. Six avaient des caractéristiques typiques de l’épilepsie myoclonique sévère du nourrisson (SMEI), alors que les six autres étaient « borderline ». Tous les douze ont subi une série d’évaluations neuropsychologiques avec des échelles de développement neurologique et une évaluation plus approfondie de certaines capacités cognitives.
RÉSULTATS: Nos résultats ont rapporté un développement apparent normal avant l’apparition de la maladie, une évolution générale en deux étapes principales, la première plus active et une tendance générale vers une stabilisation clinique par la suite. L’apparition du déclin cognitif était généralement plus tard que ce qui est rapporté dans d’autres séries, de plus, la dépréciation du développement cognitif est moins sévère, en particulier dans les cas « borderline ». Quant à la compétence cognitive spécifique, l’attention, l’intégration visuelle motrice, la perception visuelle ainsi que les fonctions exécutives sont les aptitudes les plus affaiblies; le langage apparaît moins impliqué, avec une prédominance des défauts phonologiques.
CONCLUSIONS: Dans notre cohorte, le développement global des patients semblent moins touché que dans les études précédentes. Par ailleurs, notre étude souligne une déficience de plusieurs compétences cognitives spécifiques, même chez les patients avec un quotient de développement apparemment dans la gamme normale. Le langage et d’autres troubles de compétences cognitives comme l’attention, l’organisation visuo-spatiale, la mémoire de travail et les fonctions exécutives semblent compatibles avec ce que l’on trouve habituellement dans les troubles cérébelleux.
Epilepsia. 2011 Apr;52 Suppl 2:102-4. doi: 10.1111/j.1528-1167.2011.03013.x.
The impact of parent advocacy groups, the Internet, and social networking on rare diseases: the IDEA League and IDEA League United Kingdom example.
International Dravet syndrome Epilepsy Action League, Deale, Maryland, USA. Dr.Black@IDEA-League.org
The development of the Internet and subsequent evolution of social networking has significantly changed the effectiveness of patient advocacy groups for rare diseases. The greatest degree of change has occurred at the patient level, with an increased ability of affected individuals to share experiences and support, and to raise public awareness. Other changes have occurred, not only in the way rare diseases are diagnosed, studied, and treated, but also in how they are addressed at the level of legislation and public policy. The International Dravet syndrome Epilepsy Action League (IDEA League) is the leading patient advocacy organization for Dravet syndrome and related genetic ion-channel epilepsy disorders (hereafter referred to as Dravet syndrome or severe myoclonic epilepsy of infancy, SMEI). The IDEA League’s mission encompasses international support and outreach for patients and families, as well as collaboration with physicians, medical education, health care coordination, and research. The IDEA League is an excellent example of the impact of patient advocacy groups, the Internet, and social networking on the landscape of rare diseases.
Epilepsia. 2011 Apr;52 Suppl 2:95-101. doi: 10.1111/j.1528-1167.2011.03012.x.
Dravet syndrome and parent associations: the IDEA League experience with comorbid conditions, mortality, management, adaptation, and grief.
Skluzacek JV, Watts KP, Parsy O, Wical B, Camfield P.
International Dravet syndrome Epilepsy Action League, Deale, Maryland, USA. Joan.S@IDEA-League.org
The advent of social networking via the Internet and the commercial availability of tests for SCN1A mutations permitted the rapid development and growth of parent-led associations that provide advocacy and support, as well as promote education and research regarding Dravet syndrome (DS) in the last 10 years. The International Dravet syndrome Epilepsy Action League (IDEA League) is a partnership of parents and professionals united in the purpose of creating greater awareness and understanding of DS. In 2004, parents in the IDEA League support network began to collect data from families about their children with DS in order to investigate observations that, in addition to epilepsy, many of the children seemed to share similar problems. The information gained suggests comorbid conditions and raises many hypotheses for further research. The process has led to more rigorous formal studies and an increased understanding of the clinical spectrum of DS. There is an urgent need for collaborative research, comprehensive care, and professional and family education. Mortality appears high, primarily due to sudden unexplained death in epilepsy (SUDEP) and status epilepticus (SE). Most parents wish direct discussions with their child’s physician about mortality. The high risk of death and the many other stresses related to DS result in recurrent grief and loss for patients and families and highlights their need for additional advocacy and support.
Epilepsia. 2011 Apr;52 Suppl 2:90-4. doi: 10.1111/j.1528-1167.2011.03011.x.
Comprehensive care of children with Dravet syndrome.
Department of Pediatric Neuroscience, IRCCS Foundation Neurological Institute C Besta, Milano, Italy. granata@istituto-besta.it
The comprehensive care of a patient with Dravet syndrome encompasses both the « care » and the « cure » of the patient, and requires cooperation among family, doctors, and several other specialized caregivers to search for the attainment of the best quality of life for the patients and their families. Several issues peculiar to the disease to be faced while dealing with the patient are: (1) SMEI is an « evolving » disease that appears in an otherwise healthy child with symptoms that appear and mutate throughout the course of the disease; (2) the severity of the disease is not fully predictable at onset and appears to be individual-specific; (3) the seizures are invariably drug resistant and seizure freedom is not a realistic goal; and (4) in addition to seizures many other invalidating clinical problems, including cognitive impairment, behavior disorders, and a number of comorbidities characterize the disease course. The comprehensive caring must be physician-guided and patient-centered and implies a multidisciplinary approach to be built around the children and caregivers, who need to be guided through the steps of the diagnosis, treatments, and managements of the various comorbidities.
Epilepsia. 2011 Apr;52 Suppl 2:83-9. doi: 10.1111/j.1528-1167.2011.03010.x.
The ketogenic diet for Dravet syndrome and other epileptic encephalopathies: an Italian consensus.
Veggiotti P, Burlina A, Coppola G, Cusmai R, De Giorgis V, Guerrini R, Tagliabue A, Dalla Bernardina B.
Department of Child Neurology and Psychiatry, Fondazione IRCCS Istituto Neurologico C Mondino, Pavia, Italy. pveggiot@unipv.it
Ketogenic diet is a nonpharmacologic treatment for childhood epilepsy not amenable to drugs. At the present time, two works based on national research, one in Germany and one in the United States provide international guidelines to ensure a correct management of the ketogenic diet. Our Italian collaborative study group was set up in order to formulate a consensus statement regarding the clinical management of the ketogenic diet, patient selection, pre-ketogenic diet, counseling, setting and enforcement of dietary induction of ketosis, follow-up management, and eventual discontinuation of the diet.
Epilepsia. 2011 Apr;52 Suppl 2:79-82. doi: 10.1111/j.1528-1167.2011.03009.x.
Nonpharmacologic treatments of Dravet syndrome: focus on the ketogenic diet.
Servicio de Neurología, Hospital Nacional de Pediatría Prof Dr Juan P Garrahan, Buenos Aires, Argentina. rhcaraballo@arnet.com.ar
We present an update of our experience with the ketogenic diet (KD) in patients with Dravet syndrome (DS) to evaluate the efficacy and tolerability and our short experience with vagus nerve stimulation (VNS) in the treatment of this syndrome. Between March 1, 1990 and May 31, 2007, 59 patients who met diagnostic criteria for DS were studied in our department. Twenty-four of them were placed on the KD and were followed up for a minimum of 2 years. Three patients were treated with VNS. Sixteen (66.6%) of 24 patients remained on the diet. Two patients (12.5%) became seizure free, 10 children (62.5%) had a 75-99% decrease in seizures, and the remaining 4 children (25%) had a 50-74% decrease in seizures. Six patients have been off the diet for >2 years; one of them is seizure free, two have sporadic seizures, and three, who abandoned the diet after 3 years of adhering to it, relapsed. As to the efficacy of VNS, two patients had a 50-74% decrease in seizures and in the other seizure frequency remained unchanged. The device was well tolerated in all patients without significant complications. Considering the severity and refractarity of seizures in patients with DS, the fact that 12 of 16 children who remained on the diet had a significant reduction in number of seizures shows that the KD is at present an interesting therapeutic option. VNS may be a good alternative treatment for DS.
Epilepsia. 2011 Apr;52 Suppl 2:76-8. doi: 10.1111/j.1528-1167.2011.03008.x.
The effects of stiripentol on GABA(A) receptors.
Department of Pharmacology, School of Medicine, University of South Carolina, Columbia, South Carolina 29208, USA. jfisher@uscmed.sc.edu
The anticonvulsant stiripentol (Diacomittm) has been shown to have a positive impact on control of seizures for many patients with Dravet syndrome. As with most antiepileptic drugs, stiripentol has multiple mechanisms of action. Its direct anticonvulsant activity is likely due to enhancement of inhibitory, γ-aminobutyric acid (GABA)ergic neurotransmission. Stiripentol was shown to increase the activity of both neuronal and recombinant GABA(A) receptors at clinically relevant concentrations. At recombinant receptors, stiripentol was found to act through a unique site in a subunit-dependent manner. Positive modulation by stiripentol was most effective at GABA(A) receptors containing an α3 subunit. The expression of the α3 subunit is developmentally regulated, with highest levels in the immature brain. This subunit selectivity may explain the greater clinical efficacy of stiripentol in childhood-onset epilepsies, including Dravet syndrome.
Epilepsia. 2011 Apr;52 Suppl 2:72-5. doi: 10.1111/j.1528-1167.2011.03007.x.
The pharmacologic treatment of Dravet syndrome.
Inserm, U663, Paris, France. catherine.chiron@nck.aphp.fr
Dravet syndrome (DS) is one of the most pharmacoresistant epilepsy syndromes. Valproate is used as a first-line agent to prevent the recurrence of febrile seizures and oral/nasal/rectal benzodiazepine is used for any long-lasting seizures, but these agents are most often insufficient. Lamotrigine, carbamazepine, and high doses of intravenous phenobarbital should be avoided because they may worsen seizures. Topiramate, levetiracetam, bromide, and the ketogenic diet may provide substantial efficacy as adjunctive therapy/procedure. Stiripentol is the only compound that proved its efficacy in DS through two independent randomized placebo-controlled trials, when combined with valproate and clobazam. Their dose has to be decreased to minimize the side effects (mostly loss of appetite) resulting from pharmacokinetic interactions of stiripentol powerfully inhibiting cytochromes P450. Stiripentol acts as a γ-aminobutyric acid (GABA)ergic agent, mainly via the α3 subunit of GABA(A) receptors. Stiripentol (Diacomit) was approved as an orphan drug in 2007 in Europe for adjunctive therapy in DS. Up to now, >500 children have been safely treated, and recent experiment in Japan confirmed stiripentol benefit in DS children with comedications other than valproate and clobazam. Because early status epilepticus is likely to negatively impact cognitive outcome, we recommend the introduction of stiripentol as soon as the diagnosis of DS is clinically confirmed. Topiramate and the ketogenic diet are alternatives in pharmacoresistant cases.
Epilepsia. 2011 Apr;52 Suppl 2:70-1. doi: 10.1111/j.1528-1167.2011.03006.x.
Molecular and cellular basis: insights from experimental models of Dravet syndrome.
Laboratory for Neurogenetics, RIKEN Brain Science Institute, Hirosawa 2-1, Wako-shi, Saitama, Japan. yamakawa@brain.riken.jp
Dravet syndrome is caused by mutations of the SCN1A gene that encodes voltage-gated sodium channel alpha-1 subunit. SCN1A-knock-in mouse with a disease-relevant nonsense mutation that we generated well reproduced the disease phenotypes. Both homozygous and heterozygous knock-in mice developed epileptic seizures within the first postnatal month. In heterozygotes, trains of evoked action potentials in fast-spiking, inhibitory cells exhibited pronounced spike amplitude decrement late in the burst but not in pyramidal neurons. Furthermore, our immunohistochemical studies showed that in wild-type mice Nav1.1 is expressed in parvalbumin-positive inhibitory interneurons (PV cells), dominantly in its axons and moderately in somata, and not expressed in pyramidal cells nor other types of interneurons including somatostatin-positive and calretinin-positive cells. These results so far suggest that Nav1.1 expression is largely confined to PV cells and plays critical roles in their spike output, and that impaired function of PV cells would be the cellular basis of Dravet syndrome.
Epilepsia. 2011 Apr;52 Suppl 2:62-9. doi: 10.1111/j.1528-1167.2011.03005.x.
Dravet syndrome: insights from in vitro experimental models.
Institut de Pharmacologie Moléculaire et Cellulaire, CNRS UMR6097, University of Nice-Sophia Antipolis, Valbonne, France. mantegazza@ipmc.cnrs.fr
Dravet syndrome is caused mainly by mutations of voltage-gated Na(+) channels (most of them targeting Na(V) 1.1) and in few cases by mutations of γ-aminobutyric acid (GABA)(A) receptor γ2 subunit. In vitro functional analysis has provided important information about the pathogenic mechanism of these mutations, which is in most cases consistent with reduced GABAergic inhibition and consequent hyperexcitability of neuronal circuits. However, interpretative difficulties have arisen, limiting the exploitation of the data generated with some in vitro experimental systems. I will review the functional studies of Dravet syndrome mutations that have been performed in vitro, highlighting the interpretative difficulties and the possible use of these data in the clinical practice.
Epilepsia. 2011 Apr;52 Suppl 2:59-61. doi: 10.1111/j.1528-1167.2011.03004.x.
Insights into pathophysiology and therapy from a mouse model of Dravet syndrome.
Oakley JC, Kalume F, Catterall WA.
Department of Pharmacology Neurology, University of Washington, Seattle, Washington 98195-7280, USA.
Mutations in voltage-gated sodium channels are associated with epilepsy syndromes with a wide range of severity. Complete loss of function in the Na(v) 1.1 channel encoded by the SCN1A gene is associated with severe myoclonic epilepsy in infancy (SMEI), a devastating infantile-onset epilepsy with ataxia, cognitive dysfunction, and febrile and afebrile seizures resistant to current medications. Genetic mouse models of SMEI have been created that strikingly recapitulate the SMEI phenotype including age and temperature dependence of seizures and ataxia. Loss-of-function in Na(v) 1.1 channels results in severely impaired sodium current and action potential firing in hippocampal γ-aminobutyric acid (GABA)ergic interneurons without detectable changes in excitatory pyramidal neurons. The resulting imbalance between excitation and inhibition likely contributes to hyperexcitability and seizures. Reduced sodium current and action potential firing in cerebellar Purkinje neurons likely contributes to comorbid ataxia. A mechanistic understanding of hyperexcitability, seizures, and comorbidities such as ataxia has led to novel strategies for treatment.
Epilepsia. 2011 Apr;52 Suppl 2:55-8. doi: 10.1111/j.1528-1167.2011.03003.x.
Electrical and autonomic cardiac function in patients with Dravet syndrome.
Delogu AB, Spinelli A, Battaglia D, Dravet C, De Nisco A, Saracino A, Romagnoli C, Lanza GA, Crea F.
Pediatric Cardiology Unit, Department of Pediatrics Cardiology, Università Cattolica del Sacro Cuore, Roma, Italy. abdelogu@rm.unicatt.it
Dravet syndrome (DS) is an epileptic encephalopathy related mainly to mutations in the SCN1A gene, encoding for neuronal sodium channels. Patients with DS have a high risk of sudden unexpected death in epilepsy (SUDEP). In this study we investigated whether patients with DS present abnormalities in electrical and autonomic cardiac function. To this aim we assessed ventricular repolarization and heart rate variability (HRV) on standard electrocardiography (ECG) and on 24-h ECG Holter monitoring, respectively, in 20 patients affected by DS (6.8 ± 4 years, 11 female). As age- and sex-matched control groups, we also studied 20 patients with other epileptic syndromes receiving antiepileptic drugs (ES/AED, 6.0 ± 5 years, 12 female), 20 patients with other epileptic syndromes without treatment (ES/no-AED, 6.7 ± 4 years, 10 female), and 20 healthy children (HC, 7.2 ± 5 years, 11 females). Data analysis showed that patients with DS had depressed HRV variables compared to both ES patients (ES/AED and ES/no-AED) and HC control group, whereas no significant differences in HRV variables were found between ES patients (with and without treatment) and HC. There was no significant difference between patients with DS and all the other control groups in RR intervals, QT, and QTc interval analysis. In conclusion, DS patients display an imbalance of cardiac autonomic function toward a relative predominance of adrenergic tone compared to both healthy children and patients with other forms of epilepsy, independent of antiepileptic therapy. Follow-up studies should clarify the clinical significance of this autonomic impairment and whether HRV analysis can be helpful in predicting the risk of sudden death in patients with DS.
Epilepsia. 2011 Apr;52 Suppl 2:50-4. doi: 10.1111/j.1528-1167.2011.03002.x.
Mortality in Dravet syndrome: search for risk factors in Japanese patients.
Sakauchi M, Oguni H, Kato I, Osawa M, Hirose S, Kaneko S, Takahashi Y, Takayama R, Fujiwara T.
Department of Pediatrics, Tokyo Women’s Medical University, Tokyo, Japan. sakauchi@ped.twmu.ac.jp
A questionnaire survey was conducted in Japan to investigate the causes and prevalence of death related to Dravet syndrome. The questionnaire was delivered to 246 hospitals at which physicians were treating childhood epilepsy to gain information about the total number of patients with Dravet syndrome and the prevalence of early death due to the disorder. Responses to the survey were collected from 91 hospitals, and a total of 63 of 623 patients with Dravet syndrome had died. Data from 59 of these patients were analyzed. The age at death for these patients ranged from 13 months to 24 years and 11 months, with a median age of 6 years and 8 months. The causes of mortality included sudden death in 31 patients (53%), acute encephalopathy with status epilepticus (SE) in 21 patients (36%), drowning in 6 patients (10%), and other causes in one patient (1%). The incidence of sudden death reached a first peak at 1-3 years of age and a second peak at 18 years and older. In contrast, the incidence of acute encephalopathy with SE reached a peak at 6 years of age. Seven of the 10 patients who underwent SCN1A mutation analysis exhibited positive mutations but exhibited no consistent phenotype. The prevalence of Dravet syndrome-related mortality was 10.1%. The incidence of sudden death and acute encephalopathy with SE was higher in infancy (1-3 years) and at early school ages (with a peak at 6 years), respectively. Neither the treatment nor the number of seizures was associated with any cause of mortality. Factors leading to a fatal outcome are difficult to predict.
Epilepsia. 2011 Apr;52 Suppl 2:44-9. doi: 10.1111/j.1528-1167.2011.03001.x.
Dravet syndrome: the long-term outcome.
Genton P, Velizarova R, Dravet C.
Centre Saint-Paul-Hôpital Henri Gastaut, Marseille, France. piergen@aol.com
Few studies focused on the long-term outcome of Dravet syndrome in adulthood are available in the literature, but all are concordant. In this article, we consider the outcomes of 24 patients followed at the Centre Saint-Paul, Marseille, up to the age of 50, and compare them to the patients reported in the literature. Five patients (20.8%) died, at a mean age of 24.8 years, one by status epilepticus, three by sudden unexpected death in epilepsy (SUDEP), and one of unknown cause. Epileptic seizures tend to become less frequent and less severe after childhood. Fever sensitivity (temperature variations) persists throughout the clinical course of DS, but its impact on seizure frequency and severity is milder than in infancy. Generalized convulsive seizures, mostly reported as generalized tonic-clonic seizures (GTCS), were the only seizure type observed in almost all of the patients, often with a focal onset. They are less frequent than in childhood and mostly nocturnal. Some of these major convulsive seizures have less typical aspects, for example, bilateral or asymmetric tonic posturing, followed in some cases by a tonic vibratory state or clonic movements (Oguni et al., Brain Dev 2001;23:736-748; Akiyama et al., Epilepsia 2010;51:1043-1052). Other seizures like myoclonic seizures, atypical absences, and complex partial seizures (CPS) are less common in adulthood: Among our 24 patients, only 6 had atypical absences, and one myoclonic and one complex focal seizures. Electroencephalography (EEG) also changes with age but is still multiple and heterogenous, interictally and ictally. Photosensitivity and pattern sensitivity also showed a tendency to disappear before the age of 20. Motor abnormalities are common. Cerebellar features, including ataxia, dysarthria, intention tremor, and eye movement disorder, become more prominent. Walking is markedly impaired, often due to orthopedic signs such as kyphosis, kyphoscoliosis, flat feet, or claw feet. This symptomatology was minor during childhood and worsened during and after adolescence, despite physiotherapy. Mental retardation ranged from moderate to severe, with predominance of language impairment, and some patients had a major personality disorder, labeled autistic or psychotic. Dependency in adulthood is nearly constant: Only 3 of our 24 adult patients lived independently.
Epilepsia. 2011 Apr;52 Suppl 2:39-43. doi: 10.1111/j.1528-1167.2011.03000.x.
Cognitive development in children with Dravet syndrome.
Department of Pediatric Neuroscience, IRCCS Foundation Neurological Institute C Besta, Milano, Italy. francesca.ragona@istituto-besta.it
Slowing of cognitive skills represents one of the diagnostic criteria of Dravet syndrome. This Italian multicentric study aims at clarifying the roles of epilepsy and/or underlying genetic alteration in determining the cognitive outcome. The study includes infants that were either in follow-up (retrospective study: 26 cases) and newly diagnosed (prospective study: in progress). Our multicentric study shows that slowing of cognitive achievements becomes evident during the second year of life in all cases, and that the epilepsy phenotype indeed has a prognostic value. In this study the early appearance of absences and myoclonic seizures is associated with the worst cognitive outcome; whereas convulsive prolonged seizures do not seem to represent, per se, a bad prognostic factor for mental outcome. In this study, statistical analysis failed to reveal differences in the cognitive outcome with regard to the presence and type of SCN1A mutation.
Epilepsia. 2011 Apr;52 Suppl 2:35-8. doi: 10.1111/j.1528-1167.2011.02999.x.
Cognitive and behavioral characteristics of children with Dravet syndrome: an overview.
Child Neurology and Psychiatry, Catholic University, Rome, Italy. fguzzetta@rm.unicatt.it
We report an overview on early development of children with Dravet syndrome. After a historical outline of literature data, we refer to an Italian multicentric project, partially still in course. Because in the first year of life development seems impaired in Dravet syndrome as studies on precognitive abilities would show, defects in early development of visual function were detected heralding the subsequent cognitive decline. The delay of cognitive development, due to stagnation rather than a real deterioration, begins after the second year of life, although the age of onset varies. The extreme variability of development phenotype is confirmed and widened including also cognitive decline and severity of different defects of neuropsychological abilities as well as behavioral problems, especially associated with the cognitive decline. Mechanisms underlying neurodevelopment disorders and possible role of genetics are discussed.
Epilepsia. 2011 Apr;52 Suppl 2:30-4. doi: 10.1111/j.1528-1167.2011.02998.x.
Neuroimaging and neuropathology of Dravet syndrome.
Guerrini R, Striano P, Catarino C, Sisodiya SM.
Children’s Hospital A Meyer and University of Florence, Florence, Italy. r.guerrini@meyer.it
Brain magnetic resonance imaging (MRI) studies in patients with Dravet syndrome and SCN1A mutations have shown abnormal findings in a small minority of patients. The origin of the structural abnormalities–such focal brain atrophy, cortical dysplasia, and hippocampal sclerosis–observed in some children remains unclear. There seems to be no correlation between the presence of MRI abnormalities and duration of epilepsy, age at seizure onset, or the frequency of episodes of status epilepticus having occurred early in life. Recent descriptions of Rasmussen syndrome and of the hemiconvulsion-hemiplegia syndrome in isolated patients with SCN1A mutations are of uncertain meaning but might indicate that co-occurring immunomediated or seizure-induced structural changes can, in turn, become a substrate for the severe epileptic encephalopathy. The few available neuropathologic studies of Dravet syndrome have provided inconsistent findings, including evidence of subtle brain malformation. However, the underlying dysfunction of the SCN1A gene might confer to the brain a unique profile of vulnerability whose consequences are not easily disclosed by neuropathology and require specific experimental settings to be fully appreciated. There would seem to be value in studies in animal models of these aspects, as well as prospective studies in humans, with a particular view to establishing if earlier diagnosis and efforts at seizure control may influence the development of any clinical, imaging, or pathologic deterioration.
Epilepsia. 2011 Apr;52 Suppl 2:24-9. doi: 10.1111/j.1528-1167.2011.02997.x.
The genetics of Dravet syndrome.
Marini C, Scheffer IE, Nabbout R, Suls A, De Jonghe P, Zara F, Guerrini R.
Pediatric Neurology Unit and Laboratories, Children’s Hospital A Meyer – University of Florence, Florence, Italy. c.marini@meyer.it
Dravet syndrome (DS), otherwise known as severe myoclonic epilepsy of infancy (SMEI), is an epileptic encephalopathy presenting in the first year of life. DS has a genetic etiology: between 70% and 80% of patients carry sodium channel α1 subunit gene (SCN1A) abnormalities, and truncating mutations account for about 40% and have a significant correlation with an earlier age of seizures onset. The remaining SCN1A mutations comprise splice-site and missense mutations, most of which fall into the pore-forming region of the sodium channel. Mutations are randomly distributed across the SCN1A protein. Most mutations are de novo, but familial SCN1A mutations also occur. Somatic mosaic mutations have also been reported in some patients and might explain the phenotypical variability seen in some familial cases. SCN1A exons deletions or chromosomal rearrangements involving SCN1A and contiguous genes are also detectable in about 2-3% of patients. A small percentage of female patients with a DS-like phenotype might carry PCDH19 mutations. Rare mutations have been identified in the GABARG2 and SCN1B genes. The etiology of about 20% of DS patients remains unknown, and additional genes are likely to be implicated.
Epilepsia. 2011 Apr;52 Suppl 2:13-23. doi: 10.1111/j.1528-1167.2011.02996.x.
Electroencephalographic characteristics of Dravet syndrome.
Centre Saint Paul, Hôpital Henri Gastaut, Marseille, France. michelle-bureau@wanadoo.fr
In Dravet syndrome, interictal and ictal electroencephalography (EEG) recording may remain misleading, and are not specifically altered. Moreover, there is a great polymorphism of clinical and EEG seizure types. Some can be observed in other epileptic syndromes, but others are more specific–particularly the peculiar unilateral seizures, the falsely generalized seizures, probably with a focal onset, and the unstable seizures. In some cases, the ictal manifestations are characterized by the persistent predominant recurrence of convulsive seizures, often induced by body temperature increase, eventually associated with partial complex seizures. The myoclonic events, absences with myoclonic component, obtundation status, and photosensitivity and/or pattern sensitivity are absent or appear relatively late and recur transiently for short periods. In these cases interictal EEG is characterized by the persistent paucity of paroxysmal discharges. In other cases, on a background of convulsive seizures and body temperature sensitivity, one may find a variable association of (1) myoclonic seizures of different types, (2) a strong sensitivity to light and pattern stimulations, with early onset and persistent in time. In these cases, interictal paroxysms and spontaneous and induced (intermittent photic stimulation, patterns, and eye closure) stimulation tend to appear early and to be frequent and persistent during the evolution. According to these electroclinical patterns it is possible to divide the population into two subsets, both sharing common genetic mechanisms but with a different clinical outcome.
Epilepsia. 2011 Apr;52 Suppl 2:10-2. doi: 10.1111/j.1528-1167.2011.02995.x.
Borderline Dravet syndrome: a useful diagnostic category?
Children’s Hospital A Meyer and University of Florence, Florence, Italy. r.guerrini@meyer.it
The term « borderline » severe myoclonic epilepsy of infancy (SMEIB) has been used to designate patients in whom myoclonic seizures or generalized spike and wave activity are absent. It has also been used loosely to indicate mild forms of the syndrome. It is now acknowledged that the course and outcome of patients with SMEIB are the same as in the core syndrome. The rate of patients exhibiting SCN1A gene mutations is also similar, and it has been observed that the same mutations can cause both typical and « borderline » forms, indicating causal homogeneity. Defining a borderline form of a syndrome would mean setting the criteria of semiology and severity whereby a given phenotype falls within and outside the core syndrome. Such process has never been made for Dravet syndrome and is of course unrealistic in view its polymorphic expression. The eponym Dravet syndrome has been preferred to designate a syndrome spectrum that also embraces SMEIB. Therefore the term « borderline » Dravet syndrome is improper. The definition « mild form » of Dravet syndrome would certainly be more suitable to indicate those patients exhibiting a less severe or incomplete form of the syndrome. Variability in severity favors the concept that SCN1A loss of function causes a spectrum of epilepsy phenotypes in which seizures, often prolonged and precipitated by fever, are the prominent feature and schematic subdivisions would be inappropriate, at least in the early stages. An initial definition of SCN1A gene-related epilepsy would perhaps be more suitable when a mutation of this gene is ascertained and the clinical picture is still ill defined.
Epilepsia. 2011 Apr;52 Suppl 2:3-9. doi: 10.1111/j.1528-1167.2011.02994.x.
The core Dravet syndrome phenotype.
Centre Saint-Paul-Hôpital Henri Gastaut, Marseille, France. charlotte.dravet@free.fr
Dravet syndrome was described in 1978 by Dravet (1978) under the name of severe myoclonic epilepsy in infancy (SMEI). The characteristics of the syndrome were confirmed and further delineated by other authors over the years. According to the semiologic features, two forms have been individualized: (1) the typical, core, SMEI; and (2) the borderline form, SMEIB, in which the myoclonic component is absent or subtle. Clinical manifestations at the onset, at the steady state, and during the course of the disease are analyzed in detail for the typical Dravet syndrome, and the differential diagnosis is discussed. Onset in the first year of life by febrile or afebrile clonic and tonic-clonic, generalized, and unilateral seizures, often prolonged, in an apparently normal infant is the first symptom, suggesting the diagnosis. Later on, multiple seizure types, mainly myoclonic, atypical absences, and focal seizures appear, as well as a slowing of developmental and cognitive skills, and the appearance of behavioral disorders. Mutation screening for the SCN1A gene confirms the diagnosis in 70-80% of patients. All seizure types are pharmacoresistent, but a trend toward less severe epilepsy and cognitive impairment is usually observed after the age of 5 years.
Epilepsia. 2011 Apr;52 Suppl 2:1-2. doi: 10.1111/j.1528-1167.2011.02993.x.
Severe myoclonic epilepsy in infancy (Dravet syndrome) 30 years later.
Dravet C, Bureau M, Dalla Bernardina B, Guerrini R.
Centre Saint-Paul-Hôpital Henri Gastaut, Marseille, France. charlotte.dravet@free.fr